Testicular cancer is a type of cancer that develops in the testicles, the male reproductive organs responsible for producing sperm and testosterone. While it is relatively rare compared to other types of cancer, it predominantly affects young men between the ages of 15 and 40. Despite its rarity, testicular cancer is highly treatable, especially when detected early. By understanding the basics of this condition, its risk factors, symptoms, diagnosis, and treatment options, individuals can empower themselves to take control of their health and potentially save lives.
In this blog, we will delve into the world of testicular cancer, shedding light on important aspects such as its prevalence, potential causes, and the signs and symptoms to watch out for. We will explore the diagnostic procedures used to identify this cancer and discuss the available treatment options. Additionally, we will emphasise the importance of regular self-examinations, routine medical check-ups, and the role of awareness in early detection and prevention.
Understanding testicular cancer
Anatomy and Function of the Testicles: To better understand testicular cancer, it is important to familiarize ourselves with the anatomy and function of the testicles. The testicles are two small, oval-shaped glands located inside the scrotum, which is the loose pouch of skin beneath the penis. Their primary function is to produce sperm and testosterone, the male sex hormone.
Types of Testicular Cancer
There are two main types of testicular cancer: germ cell tumours and non-germ cell tumours.
- Germ Cell Tumors: Germ cell tumours account for the majority of testicular cancer cases. They arise from the cells that produce sperm and are further classified into two subtypes:
a) Seminomas: Seminomas are slower-growing tumours that typically occur in men in their 30s and 40s. They tend to respond well to radiation therapy and chemotherapy.
b) Non-seminomas: Non-seminomas are a group of faster-growing tumours that often develop in younger men, typically in their late teens or early twenties. They are further divided into several subtypes, including embryonal carcinoma, yolk sac tumour, choriocarcinoma, and teratoma. - Non-Germ Cell Tumors: Non-germ cell tumours are less common and typically occur in older men. They can originate from various types of cells found in the testicles, such as Leydig cells, Sertoli cells, and stromal cells. Non-germ cell tumours are often treated differently from germ cell tumours, as their behaviour and response to treatment may vary.
Prevalence and Incidence Rates: Although testicular cancer accounts for a small percentage of overall cancer cases, its incidence has been increasing over the past few decades. In the United States, it is estimated that around 9,000 new cases of testicular cancer will be diagnosed each year. However, the overall survival rate for testicular cancer is high, with more than 95% of patients surviving beyond five years after diagnosis.
Common Age Groups Affected: Testicular cancer primarily affects young men, with the highest incidence occurring between the ages of 20 and 34. However, it can occur at any age, including infancy and old age, although these cases are rare. It is crucial for men of all ages to be aware of the potential signs and symptoms and to seek medical attention if any abnormalities are detected in the testicles.
Risk Factors and Causes of Testicular Cancer
While the exact cause of testicular cancer is unknown, researchers have identified several risk factors that may increase an individual’s likelihood of developing the disease. It’s important to note that having one or more risk factors does not guarantee the development of testicular cancer, and individuals without any risk factors can still be diagnosed with the disease. Understanding these risk factors can help raise awareness and prompt individuals to seek medical attention if necessary.
- Cryptorchidism (Undescended Testicles): One of the most significant risk factors for testicular cancer is cryptorchidism, in which one or both testicles fail to descend into the scrotum before birth. Men with a history of undescended testicles have a higher risk of developing testicular cancer, even if the condition was surgically corrected in childhood.
- Family History and Genetic Factors: Having a close relative, such as a father or brother, with a history of testicular cancer increases the risk. Certain genetic conditions, such as Klinefelter syndrome, where a male is born with an extra X chromosome (XXY), and Carney complex, a rare genetic disorder, have also been associated with an increased risk of testicular cancer.
- Personal History of Testicular Cancer: Men who have previously had testicular cancer are at a higher risk of developing it in the remaining testicle or in the other testicle if both were affected.
- Ethnicity and Race: Testicular cancer is more commonly diagnosed in Caucasian men compared to men of other ethnic backgrounds. Asian and African descent individuals have a lower risk, but it can still occur.
- HIV Infection: Men infected with the human immunodeficiency virus (HIV) may have a higher risk of developing testicular cancer.
- Environmental and Occupational Factors: Exposure to certain environmental and occupational factors may increase the risk of testicular cancer. These include exposure to chemicals like pesticides, herbicides, and dioxins. Additionally, men working in industries such as agriculture, construction, or mining may face a slightly higher risk due to potential exposure to harmful substances.
It’s important to note that most cases of testicular cancer occur in men without any known risk factors. Therefore, even in the absence of these risk factors, it is crucial for all men to be aware of the signs and symptoms of testicular cancer and to perform regular self-examinations.
Signs and Symptoms of Testicular Cancer
Early detection of testicular cancer is key to successful treatment and improved outcomes. Being aware of the signs and symptoms can help individuals recognize potential abnormalities in their testicles and seek medical attention promptly. It’s important to note that not all symptoms are indicative of testicular cancer, and they can vary from person to person. If any of the following signs or symptoms are experienced, it is advisable to consult a healthcare professional for further evaluation:
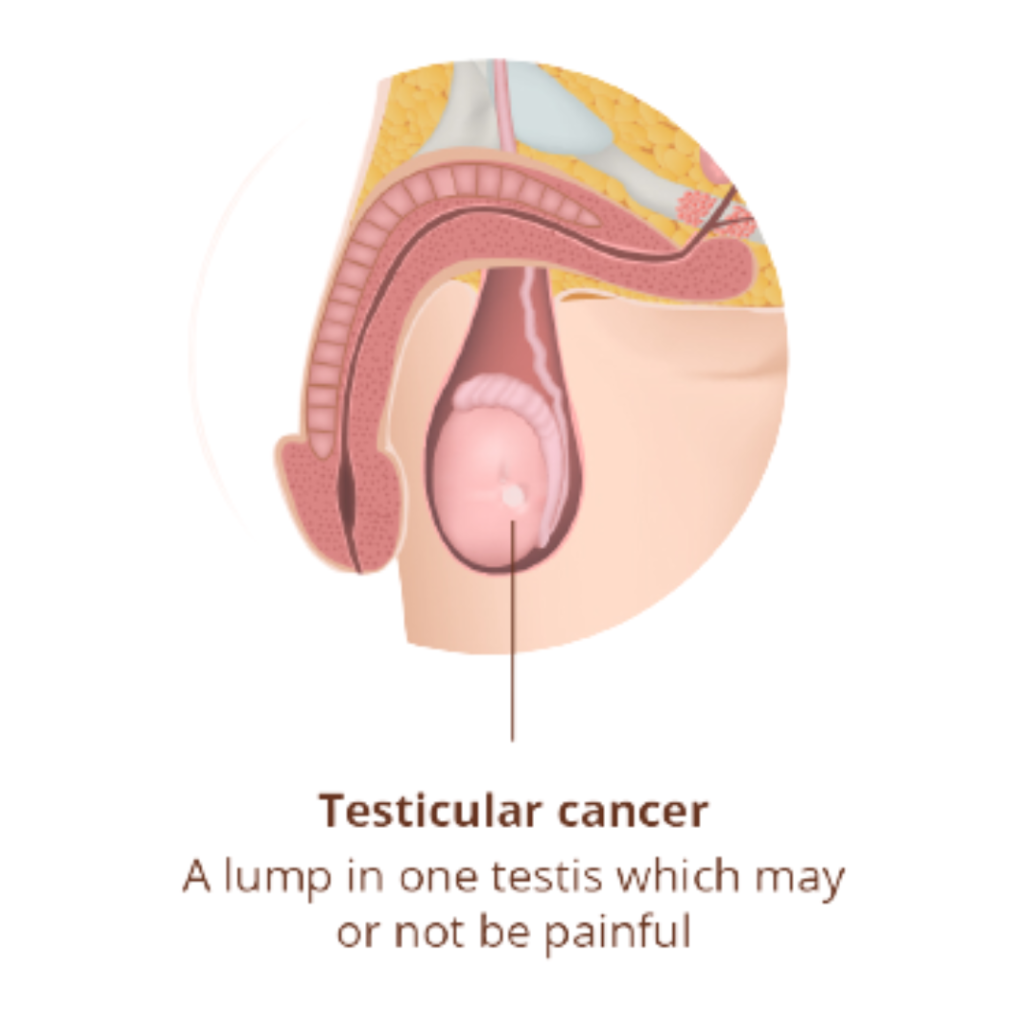
- Lump or Swelling in the Testicle: The most common sign of testicular cancer is the presence of a lump or swelling in one or both testicles. The lump may be small or large and can vary in texture (firm or soft). It is typically painless, but some individuals may experience discomfort or tenderness.
- Testicular Pain or Discomfort: Testicular pain or discomfort can occur without the presence of a lump. The pain may range from a dull ache to a sharp, intense sensation. It can affect one or both testicles and may radiate to the lower abdomen or groin area.
- Heaviness or Aching Sensation: Some individuals with testicular cancer may experience a persistent feeling of heaviness or ache in the scrotum or lower abdomen. This sensation may be present even without a visible lump.
- Changes in Testicle Size or Shape: It can cause noticeable changes in the size or shape of the testicles. One testicle may become larger or smaller than the other, or there may be a change in the overall shape or consistency of the testicle.
- Back Pain or Abdominal Pain: In some cases, testicular cancer can cause pain or discomfort in the lower back or abdomen. This may be a result of the cancer spreading to nearby lymph nodes or other organs.
- Breast Enlargement or Tenderness: In rare cases, certain types of cancer, such as choriocarcinoma, can cause hormonal changes that lead to breast enlargement (gynecomastia) or breast tenderness.
It’s important to remember that these symptoms can also be caused by conditions other than testicular cancer, such as infections or injury. However, if any of these symptoms persist for more than a couple of weeks or cause concern, it is essential to consult a healthcare professional for further evaluation and diagnosis.
Diagnosis and Staging of Testicular Cancer
When testicular cancer is suspected based on symptoms or during a physical examination, various diagnostic tests are employed to confirm the diagnosis and determine the stage of the cancer. Prompt and accurate diagnosis is crucial for developing an appropriate treatment plan. The following are common diagnostic procedures used for testicular cancer:
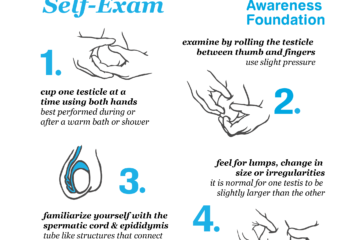
- Self-Examination and Medical Examination: A self-examination is a valuable tool for detecting testicular abnormalities. Men are encouraged to perform regular self-examinations to check for any lumps, swelling, or changes in the testicles. If any abnormalities are detected, a medical examination by a healthcare professional is necessary to further evaluate the condition.
- Imaging Tests
Ultrasound: Ultrasound is often the first imaging test performed to evaluate testicular abnormalities. It uses sound waves to create detailed images of the testicles, helping identify the presence, size, location, and characteristics of any masses or tumours.
Computed Tomography (CT) Scan: CT scans may be conducted to determine if the cancer has spread to the lymph nodes, abdomen, or other organs. It provides detailed cross-sectional images of the body.
Magnetic Resonance Imaging (MRI): MRI may be utilized to obtain detailed images of the testicles and surrounding tissues, providing additional information about the extent of the cancer.
- Blood Tests: Tumor markers are substances present in the blood that can be elevated in the presence of certain types of testicular cancer. The two primary tumour markers for testicular cancer are alpha-fetoprotein (AFP) and human chorionic gonadotropin (HCG). Blood tests for these markers are often conducted to help diagnose testicular cancer, monitor treatment response, and detect any potential recurrence.
- Biopsy and Pathology Examination: If a testicular mass is detected, a biopsy may be performed to collect a tissue sample for further examination. In the case of suspected testicular cancer, radical inguinal orchiectomy is usually recommended as the initial treatment, which involves the surgical removal of the affected testicle. The removed testicle is sent to a pathology laboratory where it is examined under a microscope to determine the presence of cancer cells and their type.
- Staging: Staging is a process that helps determine the extent and spread of cancer. The stage of cancer is important for selecting the appropriate treatment approach. Testicular cancer is typically staged using the TNM system, which considers the size of the tumour (T), involvement of lymph nodes (N), and presence of distant metastasis (M). Further staging may be determined based on additional factors such as tumour markers and histology.
The staging of testicular cancer can range from Stage I (localized cancer) to Stage IV (advanced cancer with distant metastasis). The specific staging information guides the treatment decisions and prognosis for the individual.
Treatment Options for Testicular Cancer
The treatment depends on various factors, including the stage and type of cancer, the presence of any tumour markers, and the overall health of the individual. The primary treatment options for testicular cancer include surgery, radiation therapy, and chemotherapy. In some cases, a combination of these treatments may be recommended. The treatment plan is typically determined by a multidisciplinary team of healthcare professionals, including urologists, medical oncologists, and radiation oncologists. Let’s explore the different treatment options in more detail:
- Surgery:
Radical Inguinal Orchiectomy: The first step in treating testicular cancer is often the surgical removal of the affected testicle, a procedure called radical inguinal orchiectomy. This surgery involves removing the entire testicle through an incision in the groin. If the cancer is confined to one testicle, removal of the affected testicle may be curative.
Retroperitoneal Lymph Node Dissection (RPLND): In some cases, when there is evidence of lymph node involvement or to prevent recurrence, a retroperitoneal lymph node dissection may be performed. This surgery involves removing the lymph nodes in the abdomen to determine if the cancer has spread and to prevent its further spread.
- Radiation Therapy: Radiation therapy uses high-energy beams to kill cancer cells or prevent their growth. It may be employed in cases where cancer has spread to the lymph nodes or as adjuvant therapy after surgery. Radiation therapy is targeted to specific areas, and treatment duration and frequency are determined based on the individual’s condition.
- Chemotherapy: Chemotherapy uses powerful medications to destroy cancer cells throughout the body. It is commonly used for testicular cancer, especially in cases where the cancer has spread beyond the testicles or in high-risk situations. Chemotherapy may involve a combination of different drugs and is typically administered in cycles over several weeks or months.
- High-Dose Chemotherapy and Stem Cell Transplant: In some advanced cases or when cancer does not respond to standard chemotherapy, high-dose chemotherapy may be utilized. High-dose chemotherapy aims to destroy the cancer cells more aggressively, but it also damages the bone marrow. To counter this, a stem cell transplant may be performed to replenish the healthy bone marrow.
- Surveillance: In certain cases, such as early-stage testicular cancer with a low risk of recurrence, a surveillance approach may be taken. Regular follow-up appointments, including physical examinations, blood tests, and imaging studies, are conducted to monitor for any signs of recurrence. If recurrence is detected, appropriate treatment is initiated.
It’s important to note that the choice of treatment depends on various factors, and the healthcare team will tailor the treatment plan to each individual’s specific situation. Treatment decisions also consider factors such as fertility preservation options, individual preferences, and overall health.
Conclusion
Testicular cancer is a relatively rare but highly treatable cancer that primarily affects young men. Early detection plays a critical role in successful treatment outcomes, making it important for individuals to be aware of the signs and symptoms of testicular cancer and to perform regular self-examinations. Consulting a healthcare professional if any abnormalities are detected is crucial.
With advancements in medical technology and treatment approaches, the prognosis for testicular cancer is generally favourable, with high survival rates. By raising awareness, promoting early detection, and supporting ongoing research, we can continue to improve outcomes and provide better care for individuals affected by testicular cancer.
Remember, if you have any concerns about testicular health or suspect any abnormalities, consult a healthcare professional for proper evaluation and guidance. Your health and well-being are worth prioritizing.
Dr. Sumit Sharma is an experienced urologist, andrologist, and kidney transplant surgeon with over 20 years of clinical experience. He is the founder of the Department of Urology at multiple hospitals in Gurgaon and has established successful kidney transplant programs across the city.