Living with an overactive bladder (OAB) can be challenging and disruptive to one’s daily life. OAB is a common condition characterized by a sudden, frequent, and uncontrollable urge to urinate. It can significantly impact an individual’s quality of life, leading to anxiety, embarrassment, and limitations in social activities. However, there are several strategies and lifestyle modifications that can help individuals effectively manage their symptoms and regain control over their lives. By incorporating these tips into their daily routine, individuals with OAB can experience a significant reduction in the frequency and urgency of bathroom visits, allowing them to lead a more comfortable and active lifestyle. In this blog, we will explore various tips and techniques for managing OAB, empowering you with the knowledge to better understand and cope with this condition.
Understanding Overactive Bladder
Overactive bladder (OAB) is a common medical condition that affects millions of people worldwide. It refers to a set of symptoms characterized by an urgent and frequent need to urinate, often accompanied by an inability to control bladder function. Individuals with OAB may experience sudden and intense urges to urinate, even when the bladder is not full, leading to involuntary urine leakage, known as urge incontinence.
Symptoms of Overactive Bladder:
- Urinary urgency: A sudden and compelling need to urinate that is difficult to control.
- Frequency: The need to urinate more frequently than normal, often exceeding eight times a day.
- Nocturia: Waking up during the night to urinate, disrupts sleep patterns.
- Urge incontinence: Involuntary leakage of urine following a strong urge to urinate.
Causes and Risk Factors:
The exact cause of OAB is not fully understood, but several factors can contribute to its development. These include:
- Bladder muscle dysfunction: Overactive bladder can occur when the muscles of the bladder contract involuntarily, creating a sense of urgency and frequent urination.
- Nerve abnormalities: Issues with the nerves that control bladder function can disrupt communication between the brain and the bladder, leading to OAB symptoms.
- Age: OAB becomes more prevalent with age, as bladder muscles and nerves may weaken over time.
- Gender: OAB is more common in women than in men, possibly due to factors such as pregnancy, childbirth, and hormonal changes.
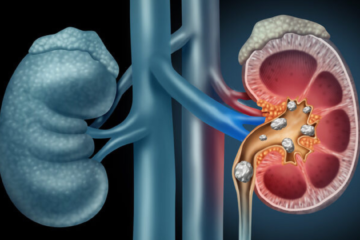
- Medical conditions: Certain medical conditions, such as urinary tract infections, bladder stones, and neurological disorders (e.g., multiple sclerosis), can contribute to OAB symptoms.
- Lifestyle factors: Excessive fluid intake, caffeine consumption, obesity, and chronic constipation can increase the risk of developing OAB.
Differentiating OAB from Other Urinary Conditions:
It is important to differentiate OAB from other urinary conditions that may present similar symptoms. Some conditions that may be mistaken for OAB include:
- Urinary tract infections (UTIs): UTIs can cause urgency and frequency of urination, but they are typically accompanied by other symptoms such as pain or burning during urination.
- Stress incontinence: Stress incontinence is the leakage of urine during activities that put pressure on the bladder, such as laughing, sneezing, or exercising. It differs from OAB as the urgency component is absent.
- Mixed incontinence: Some individuals may experience a combination of OAB symptoms (urgency, frequency) and stress incontinence (leakage with exertion).
It is important to consult with a healthcare professional for an accurate diagnosis and appropriate treatment plan.
In the next sections of this blog, we will explore various tips and strategies for managing an overactive bladder, including lifestyle modifications, behavioural strategies, and medical interventions. These approaches can help individuals effectively manage their symptoms and improve their overall quality of life.
Tips and Strategies for Managing Overactive Bladder
Living with an overactive bladder (OAB) can be challenging, but there are various tips and strategies that can help individuals effectively manage their symptoms. By incorporating these approaches into daily life, individuals with OAB can experience a significant reduction in the frequency and urgency of bathroom visits, allowing them to regain control and improve their quality of life. Here are some tips and strategies for managing an overactive bladder:
- Fluid Management:
- Monitor and adjust fluid intake: Pay attention to the amount and timing of fluids consumed throughout the day. It may be helpful to keep a bladder diary to track fluid intake and identify patterns that trigger symptoms.
- Identify bladder irritants to avoid: Certain beverages and foods can irritate the bladder and worsen OAB symptoms. Common irritants include caffeine, alcohol, carbonated drinks, spicy foods, and artificial sweeteners. Limit or avoid these triggers.
- Dietary Changes:
- Eliminate or reduce certain food and drinks: In addition to bladder irritants, some individuals may find that specific foods, such as citrus fruits, tomatoes, chocolate, and acidic or highly spiced dishes, exacerbate their OAB symptoms. Experiment with eliminating or reducing these items from your diet to see if it makes a difference.
- Incorporate bladder-friendly foods: Some foods, on the other hand, may have a positive impact on bladder health. These include foods high in fibre (to prevent constipation), fruits and vegetables, lean proteins, and foods rich in antioxidants and vitamins.
- Bladder Training:
- Scheduled voiding techniques: Establish a regular bathroom schedule, even if you don’t feel the urge to urinate. Gradually increase the time between bathroom visits by a few minutes each week. This helps retrain the bladder and increase its capacity.
- Gradually increase the time between bathroom visits: Practice holding urine for progressively longer intervals to help increase bladder capacity and reduce the frequency of bathroom trips.
- Pelvic Floor Exercises:
- Strengthening pelvic floor muscles with Kegel exercises: These exercises involve contracting and relaxing the muscles used to control urine flow. Strengthening the pelvic floor can help improve bladder control and reduce symptoms of OAB. Consult a healthcare professional or a pelvic floor therapist for guidance on performing Kegel exercises correctly.
- Behavioural Strategies:
- Urge suppression techniques: When you feel the urge to urinate, practice relaxation techniques such as deep breathing, distraction techniques (e.g., counting backwards from 100), and visualization exercises to help calm the bladder and suppress the urge temporarily.
- Double voiding: Empty your bladder completely by urinating, waiting a few minutes, and then trying to urinate again. This can help ensure that the bladder is fully emptied, reducing the risk of urge incontinence.
- Medical Interventions:
- Medications for OAB: There are various medications available that can help relax the bladder muscles and reduce OAB symptoms. These medications work in different ways, such as reducing muscle contractions or increasing bladder capacity. Consult a healthcare professional to discuss medication options, potential side effects, and suitability for your specific situation.
- Botox injections: In severe cases of OAB that do not respond to other treatments, Botox injections can be considered. Botox helps relax the bladder muscles and reduce the frequency of contractions. This is a procedure performed by a healthcare professional and requires regular re-treatment.
- Nerve stimulation: Sacral nerve stimulation (SNS) and percutaneous tibial nerve stimulation (PTNS) are minimally invasive procedures that involve stimulating specific nerves to help regulate bladder function. These treatments are typically recommended for individuals who have not responded to other treatments or medications.
Remember, it is essential to consult with a healthcare professional to discuss the most suitable treatment options for your specific situation. They can provide personalized guidance and recommendations based on your symptoms and medical history.
Incorporating these tips and strategies into your daily routine can help you effectively manage overactive bladder symptoms and improve your overall quality of life. Experiment with different approaches to find what works best for you, and don’t hesitate to seek support from healthcare professionals or support groups specializing in OAB management. You don’t have to let OAB control your life – take control and regain your independence.
Conclusion
It is important to remember that managing OAB is a personalized journey, and what works for one person may not work for another. It may require some trial and error to find the right combination of strategies that work best for you. Additionally, don’t hesitate to seek guidance from healthcare professionals who specialize in OAB management. They can provide personalized advice, recommend appropriate treatments, and address any concerns you may have.
Remember, you are not alone in your journey. There are support groups, online communities, and resources available that can provide valuable information and emotional support. Take control of your overactive bladder, implement these tips, and live your life to the fullest. You deserve to enjoy a life free from the limitations of OAB.
Dr. Sumit Sharma is an experienced urologist, andrologist, and kidney transplant surgeon with over 20 years of clinical experience. He is the founder of the Department of Urology at multiple hospitals in Gurgaon and has established successful kidney transplant programs across the city.