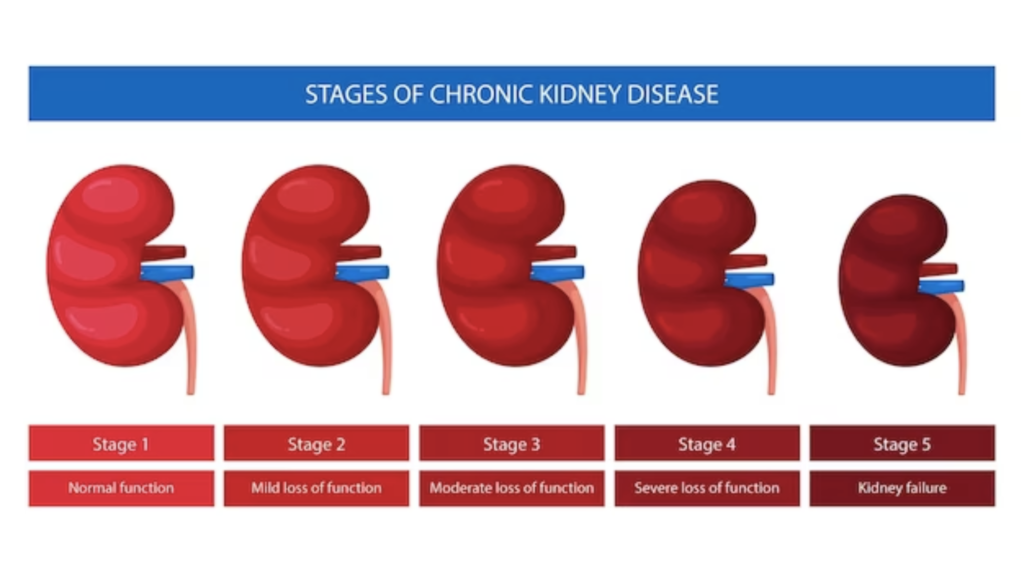
Within the complex view of human health, Chronic Kidney Disease (CKD) stands as a silent protagonist, affecting millions worldwide. As we mark its existence, what better way to delve into the complexities of medical science than by unravelling the stages of CKD? This journey takes us through the intricate web of kidney health, shedding light on the stages, causes, and strategies for managing this often-overlooked condition.
Join us as we embark on a comprehensive exploration of the stages of CKD, from its subtle inception to the critical juncture of End-Stage Renal Disease (ESRD). Together, we’ll decipher the clues that these stages provide, understanding the nuances of CKD and empowering ourselves with the knowledge that can make a significant impact on our well-being. It’s time to demystify the enigma of Chronic Kidney Disease and illuminate the path towards proactive health management.
Stage 1: Kidney Damage with Normal or Increased GFR
Stage 1 of Chronic Kidney Disease (CKD) is characterized by kidney damage with a normal or increased glomerular filtration rate (GFR). In this early stage, individuals may not experience noticeable symptoms, and the condition is often detected through routine medical check-ups or screening tests. Despite the lack of overt signs, Stage 1 CKD is a crucial point in the disease progression, as it provides an opportunity for early intervention and management.
Understanding Kidney Damage
Causes
Hypertension (High Blood Pressure): Prolonged high blood pressure can strain the blood vessels in the kidneys, leading to damage even when GFR is normal.
Diabetes Mellitus: Uncontrolled diabetes can damage the small blood vessels in the kidneys, contributing to kidney damage.
Infections or Inflammation: Conditions such as glomerulonephritis, which involve inflammation of the kidney’s filtering units, can lead to kidney damage.
Obstruction: Blockages in the urinary tract, such as kidney stones, can cause damage to the kidneys.
Diagnostic Tools
Blood Tests: Elevated levels of creatinine or decreased estimated GFR may indicate kidney dysfunction.
Urinalysis: The presence of protein or blood in the urine may signal kidney damage.
Imaging Studies: Ultrasound or other imaging techniques can help visualize the structure of the kidneys and identify abnormalities.
Normal or Increased GFR
Glomerular Filtration Rate (GFR)
The GFR is a key indicator of kidney function, representing the rate at which the kidneys filter waste from the blood. In Stage 1 CKD, despite the presence of kidney damage, the GFR remains normal or may even be increased. This means that the kidneys can still adequately perform their filtration function.
Importance of Early Detection
Opportunity for Intervention: Detecting CKD in its early stages provides a window of opportunity for healthcare professionals to address the underlying causes and implement strategies to slow or halt the progression of the disease.
Prevention of Complications: Early intervention can help prevent or manage complications associated with CKD, such as cardiovascular issues or electrolyte imbalances.
Lifestyle Modifications: Patients diagnosed with Stage 1 CKD are often advised to make lifestyle changes, including adopting a healthy diet, maintaining regular exercise, and managing blood pressure and diabetes if applicable.
Management Strategies
Blood Pressure Control: Maintaining optimal blood pressure is crucial to prevent further damage to the kidneys.
Diabetes Management: For individuals with diabetes, tight blood sugar control is essential to minimize kidney damage.
Lifestyle Changes: Adopting a healthy lifestyle, including a balanced diet low in sodium and saturated fats, can contribute to overall kidney health.
Regular Monitoring: Routine follow-up appointments and monitoring of kidney function help track changes and guide further interventions as needed.
Stage 2: Kidney Damage with Mild Decrease in GFR
Stage 2 of Chronic Kidney Disease (CKD) marks a progression from Stage 1, where there is still kidney damage, but now with a mild decrease in the glomerular filtration rate (GFR). In this stage, individuals may start to experience subtle symptoms, and it becomes even more critical to address the underlying causes and implement management strategies.
Understanding Stage 2 CKD
Causes and Risk Factors
Continued Hypertension: Uncontrolled high blood pressure remains a significant contributor to kidney damage.
Persistent Diabetes: Individuals with diabetes continue to be at risk for kidney complications, leading to the progression of CKD.
Inflammatory Conditions: Conditions causing persistent inflammation, such as autoimmune disorders or infections, can contribute to kidney damage.
Genetic Factors: Inherited conditions affecting kidney function may become more apparent in this stage.
Mild Decrease in GFR
Glomerular Filtration Rate (GFR)
While GFR remains a crucial measure, in Stage 2 CKD, there is a mild decrease in this rate. GFR values typically range between 60 and 89 millilitres per minute per 1.73 square meters, indicating a reduced ability of the kidneys to filter waste from the blood.
Symptoms
Fatigue: Individuals may start experiencing mild fatigue due to the kidneys’ reduced ability to remove waste products.
Swelling (Edema): Fluid retention may lead to swelling in the ankles, feet, or hands.
Changes in Urination: Some individuals may notice changes in urine output, such as increased frequency or foamy urine.
Importance of Early Intervention
Slowing Progression: Addressing the underlying causes, such as hypertension or diabetes, becomes even more critical to slow down the progression of CKD.
Lifestyle Modifications: Emphasizing lifestyle changes, including a renal-friendly diet and regular exercise, is crucial to support overall kidney health.
Medication Adjustments: Medications may need to be adjusted to manage blood pressure, blood sugar, or other contributing factors more effectively.
Patient Education: Educating individuals about their condition becomes increasingly important, empowering them to actively participate in their care and make informed decisions.
Long-Term Outlook
While Stage 2 CKD represents a progression in the disease, it is still a stage where proactive measures can significantly impact the long-term outlook. With proper management, individuals can lead fulfilling lives and potentially delay the need for more advanced interventions such as dialysis or kidney transplantation.
Stage 3: Moderate Decrease in GFR
Stage 3 of Chronic Kidney Disease (CKD) represents a more significant progression, characterized by a moderate decrease in the glomerular filtration rate (GFR). As kidney function continues to decline, individuals may experience noticeable symptoms, making it crucial to address the underlying causes and implement targeted management strategies.
Understanding Stage 3 CKD
Causes and Contributing Factors
Hypertension (Persistent High Blood Pressure): Uncontrolled blood pressure remains a primary contributor to kidney damage.
Diabetes Mellitus: Individuals with diabetes face an increased risk of progressive kidney dysfunction.
Glomerulonephritis: Ongoing inflammation of the kidney’s filtering units contributes to damage.
Polycystic Kidney Disease (PKD): Inherited conditions like PKD can lead to the formation of cysts, impacting kidney function.
Diagnostic Measures
Blood Tests: Creatinine levels rise further, and the estimated GFR falls into the range of 30-59 mL/min/1.73 m².
Urinalysis: Proteinuria (presence of protein in the urine) may become more pronounced, indicating ongoing kidney damage.
Imaging Studies: Imaging, such as CT scans or MRIs, may be performed to assess kidney structure and identify abnormalities.
Moderate Decrease in GFR
Glomerular Filtration Rate (GFR)
In Stage 3 CKD, the GFR falls within the range of 30-59 mL/min/1.73 m². This signifies a moderate decline in kidney function, indicating a decreased ability to filter waste products from the blood effectively.
Symptoms
Fatigue and Weakness: Increased accumulation of waste products can lead to persistent fatigue and weakness.
Fluid Retention (Edema): Swelling, particularly in the ankles and legs, may become more pronounced.
Changes in Urination: Individuals may experience changes in urine output, colour, or frequency.
Anaemia: A decline in kidney function can lead to decreased production of erythropoietin, contributing to anaemia.
Management Strategies
Blood Pressure Control: Tight control of blood pressure is crucial to slow the progression of CKD.
Diabetes Management: For individuals with diabetes, optimizing blood sugar levels is paramount in managing CKD.
Medication Adjustments: Medications to manage blood pressure, anaemia, and other symptoms may be prescribed or adjusted.
Dietary Modifications: A renal-friendly diet, low in sodium and protein, becomes more important in supporting kidney function.
Regular Monitoring: Frequent monitoring of kidney function, blood pressure, and other relevant parameters is essential for ongoing management.
Long-Term Outlook
While Stage 3 CKD signifies a more advanced stage, it is still possible to manage the condition effectively with the right interventions. Proactive measures, lifestyle modifications, and ongoing medical care can significantly impact the long-term outlook, potentially delaying the progression to more advanced stages.
Stage 4: Severe Decrease in GFR
Stage 4 of Chronic Kidney Disease (CKD) represents a substantial progression, characterized by a severe decrease in the glomerular filtration rate (GFR). At this stage, kidney function is significantly impaired, leading to more pronounced symptoms and a heightened need for targeted management and medical intervention.
Understanding Stage 4 CKD
Causes
Hypertension (Persistent High Blood Pressure): Uncontrolled blood pressure continues to be a major contributor to progressive kidney damage.
Diabetes Mellitus: Individuals with diabetes face an increased risk of severe kidney dysfunction.
Glomerulonephritis: Ongoing inflammation of the glomeruli further contributes to kidney damage.
Polycystic Kidney Disease (PKD): Inherited conditions like PKD lead to the formation of cysts, exacerbating kidney dysfunction.
Diagnostic Measures
Blood Tests: Creatinine levels rise significantly, and the estimated GFR falls below 30 mL/min/1.73 m².
Urinalysis: Proteinuria and other urinary abnormalities may become more pronounced.
Imaging Studies: Imaging techniques, such as CT scans or MRIs, may reveal structural abnormalities and the extent of kidney damage.
Severe Decrease in GFR
Glomerular Filtration Rate (GFR)
In Stage 4 CKD, the GFR falls below 30 mL/min/1.73 m², indicating a severe decline in kidney function. At this stage, the kidneys struggle to effectively filter waste products from the blood.
Symptoms
Severe Fatigue and Weakness: Accumulation of waste products results in profound fatigue and weakness.
Pronounced Edema (Swelling): Fluid retention leads to significant swelling, particularly in the extremities and around the eyes.
Changes in Urination: Urine output may decrease, and individuals may experience discomfort during urination.
Anaemia: Severe kidney dysfunction further contributes to anaemia, requiring additional interventions.
Bone Disease: Calcium and phosphorus imbalances can lead to bone problems, including bone pain and fractures.
Management Strategies
Nephrology Consultation: Individuals with Stage 4 CKD typically require specialized care from a nephrologist, who can devise tailored treatment plans.
Dialysis Evaluation: As kidney function declines, the need for renal replacement therapy, such as dialysis, is often evaluated.
Medication Adjustments: Medications to manage symptoms, blood pressure, and anaemia are carefully adjusted.
Dietary Modifications: Strict adherence to a renal-friendly diet, with limited protein, phosphorus, and sodium intake, becomes crucial.
Long-Term Outlook
Stage 4 CKD signifies a critical stage in the disease progression, demanding comprehensive care and attention. While the severity of kidney dysfunction poses challenges, appropriate management, including dialysis or kidney transplantation, can significantly enhance the quality of life and potentially prolong survival.
Stage 5: Kidney Failure (End-Stage Renal Disease)
Stage 5, also known as Kidney Failure or End-Stage Renal Disease (ESRD), represents the most advanced stage of Chronic Kidney Disease (CKD). At this point, the kidneys have experienced a profound and irreversible decline in function, necessitating renal replacement therapy for the individual to survive. Understanding the characteristics, symptoms, and management strategies for Stage 5 CKD is crucial in providing comprehensive care for those facing this challenging condition.
Characteristics of Stage 5 CKD
Glomerular Filtration Rate (GFR)
In Stage 5 CKD, the glomerular filtration rate (GFR) falls below 15 mL/min/1.73 m². This indicates a critical reduction in the kidney’s ability to filter waste products from the blood.
Complete Kidney Failure: The kidneys can no longer maintain the balance of electrolytes, remove waste products, or regulate fluid balance adequately.
Symptoms
Profound Fatigue and Weakness: The accumulation of toxins and metabolic waste products leads to severe fatigue.
Persistent Edema (Swelling): Swelling becomes extensive, affecting multiple areas of the body.
Marked Decrease in Urine Output: Individuals may experience minimal or no urine production.
Severe Anaemia: Anaemia becomes more pronounced, requiring aggressive management.
Neurological Symptoms: Cognitive impairment, confusion, and seizures may occur due to uremic encephalopathy.
Cardiovascular Complications: Individuals are at heightened risk of cardiovascular events, including heart failure.
Renal Replacement Therapy Options
Dialysis: Hemodialysis or peritoneal dialysis becomes necessary to perform the vital functions that the kidneys can no longer carry out.
Kidney Transplantation: Kidney transplantation is considered the optimal treatment for ESRD, offering the potential for a better quality of life.
Hemodialysis
Mechanism: In hemodialysis, blood is circulated through a machine that filters out waste products and excess fluids before returning the blood to the body.
Frequency: Typically performed several times a week, with each session lasting several hours.
Peritoneal Dialysis
Mechanism: Peritoneal dialysis uses the lining of the abdominal cavity (peritoneum) to filter waste and excess fluids.
Frequency: This can be performed daily at home, offering more flexibility compared to hemodialysis.
Challenges of Stage 5 CKD
Psychosocial Impact: Coping with the emotional and psychological challenges of ESRD can be overwhelming. Support from healthcare professionals, family, and mental health services is crucial.
Financial Considerations: The cost of ongoing dialysis treatments, medications, and potential transplantation can pose significant financial burdens.
Nutritional Management: Maintaining proper nutrition while adhering to dietary restrictions is essential in managing symptoms and supporting overall health.
Conclusion
Understanding the stages of CKD is not merely a journey through pathology; it is a journey through the complexities of the human body, the impact of lifestyle choices, and the importance of timely interventions. Whether we find ourselves in the early stages, where kidney damage is present but often unnoticed, or in the advanced stages, where renal replacement therapy becomes a lifeline, the key lies in knowledge, awareness, and proactive healthcare.
May this journey through the stages of CKD serve as a reminder that, in the face of health challenges, knowledge is our ally, early detection is our shield, and collaborative care is our strength. Here’s to informed decisions, resilient spirits, and a future where the stages of CKD become chapters of hope and progress.
Dr. Sumit Sharma is an experienced urologist, andrologist, and kidney transplant surgeon with over 20 years of clinical experience. He is the founder of the Department of Urology at multiple hospitals in Gurgaon and has established successful kidney transplant programs across the city.
With a commitment to the highest standards, Dr. Sumit Sharma ensures personalised, professional treatment, making your well-being the primary focus. Choose Dr. Sumit Sharma for outstanding Urological care in Gurgaon.



