The male reproductive system is a marvel of nature, finely tuned to perform its vital role in creating new life. However, like any intricate machinery, it can encounter obstacles and malfunctions that disrupt its functions. One such challenge that men may face is prostatitis, an inflammation of the prostate gland. While prostatitis can bring about a myriad of discomforts and concerns, this blog focuses on a critical aspect—its impact on male fertility.
Fertility is a deeply personal and cherished aspect of life for many individuals and couples. It represents the potential to create and nurture a new generation, and anything that threatens this ability can be a source of profound concern. Prostatitis, with its varying types and manifestations, can indeed raise questions and worries about its effects on male fertility. In this blog, we embark on a journey to understand prostatitis comprehensively, exploring its types, causes, symptoms, and, most importantly, its intricate relationship with male fertility. We’ll delve into the science behind this condition, debunk myths, and provide valuable insights to empower you with the knowledge needed to make informed decisions about your reproductive health.
Types of Prostatitis
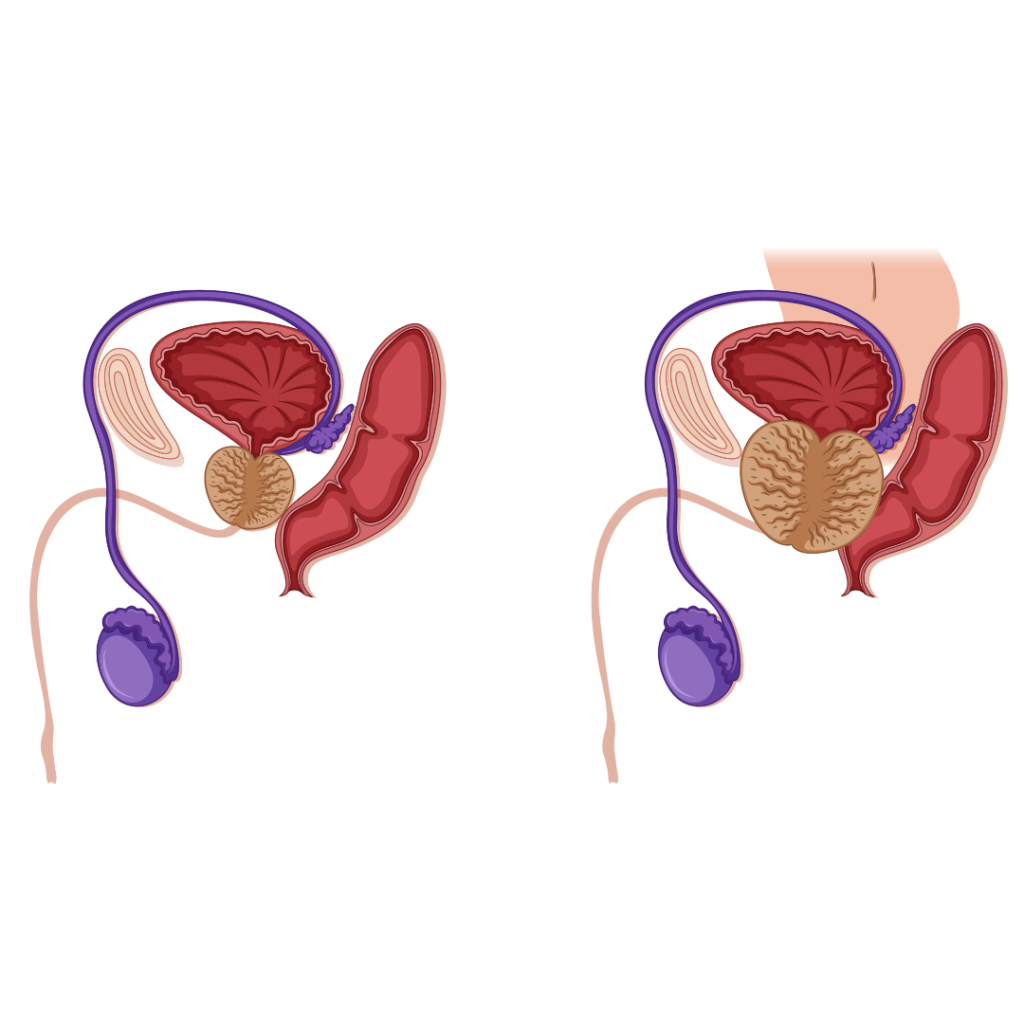
Prostatitis is a urological condition characterized by the inflammation of the prostate gland, a small, walnut-sized organ located just below the bladder. Understanding the different types of prostatitis is essential as each type presents with distinct characteristics, causes, and symptoms. In this section, we will delve into the four primary types of prostatitis:
- Acute Bacterial Prostatitis (ABP)
ABP is the result of a bacterial infection in the prostate gland. Bacteria, typically from the urinary tract or elsewhere in the body, invade the prostate tissue, leading to inflammation.
- Chronic Bacterial Prostatitis (CBP)
CBP, as the name suggests, is a long-term bacterial infection of the prostate gland. It differs from ABP in that the symptoms are less severe and may come and go over an extended period.
- Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS)
CP/CPPS is the most common form of prostatitis, and its exact cause is often elusive. While it is not primarily bacterial, some researchers believe it may be related to inflammation, autoimmune reactions, or nerve dysfunction.
- Asymptomatic Inflammatory Prostatitis (AIP)
AIP is often discovered incidentally during medical evaluations for other conditions. It is characterized by the presence of inflammation in the prostate without noticeable symptoms.
Understanding the differences between these four types of prostatitis is crucial for accurate diagnosis and appropriate treatment. Each type has its unique challenges and management strategies, and consulting with a healthcare professional is essential if you suspect you have prostatitis or are experiencing related symptoms.
Causes and Risk Factors of Prostatitis
Prostatitis is a condition characterized by inflammation of the prostate gland, which can lead to a variety of symptoms and discomfort. Understanding the causes and risk factors associated with prostatitis is crucial for prevention and effective management. In this section, we’ll explore the factors that can contribute to the development of prostatitis in detail:
1. Bacterial Infections
- Cause: Bacterial prostatitis, including acute bacterial prostatitis (ABP) and chronic bacterial prostatitis (CBP), is primarily caused by the invasion of bacteria into the prostate gland. Common bacteria responsible for these infections include Escherichia coli (E. coli), Klebsiella, and Proteus species.
- Risk Factors:
- Urinary Tract Infections (UTIs): A history of recurrent UTIs can increase the risk of bacterial prostatitis as bacteria from the urinary tract may travel into the prostate.
- Instrumentation: Procedures involving the urinary tract, such as catheterization or cystoscopy, can introduce bacteria into the prostate, leading to infection.
- Incomplete Emptying of the Bladder: Incomplete voiding of the bladder can allow bacteria to accumulate in the urinary tract and potentially enter the prostate.
2. Non-Bacterial Causes (Chronic Prostatitis/Chronic Pelvic Pain Syndrome – CP/CPPS)
- Cause: The exact cause of CP/CPPS is often unclear, but it is believed to be non-bacterial in origin. Possible contributing factors include inflammation, autoimmune responses, nerve dysfunction, or muscle spasms in the pelvic area.
- Risk Factors:
- Age: CP/CPPS is more commonly seen in men between the ages of 30 and 50, although it can affect men of all ages.
- Stress: Psychological stress and anxiety may exacerbate symptoms or contribute to the development of CP/CPPS.
- Pelvic Trauma: Prior pelvic trauma, such as injuries or accidents, may increase the risk of developing CP/CPPS.
3. Urinary Tract Abnormalities:
- Cause: Structural abnormalities in the urinary tract can create conditions conducive to prostatitis. These abnormalities may include urethral strictures, urethral diverticula, or conditions that obstruct the normal flow of urine.
- Risk Factors:
- Congenital Anomalies: Some individuals are born with urinary tract abnormalities that may predispose them to prostatitis.
- Prior Surgeries: Surgical procedures involving the urinary tract or nearby organs can result in scar tissue or anatomical changes that increase the risk.
4. Sexual Activity:
- Cause: Frequent or vigorous sexual activity, particularly if it leads to inadequate lubrication, can potentially irritate the prostate and contribute to prostatitis.
- Risk Factors:
- Sexual Practices: Specific sexual practices, such as prolonged or rough intercourse without sufficient lubrication, may increase the risk.
- Sexually Transmitted Infections (STIs): Certain STIs can cause urethritis, which can facilitate the spread of bacteria to the prostate.
5. Age and Family History:
- Risk Factors: While prostatitis can affect men of all ages, it is more commonly seen in men over 30. Having a family history of prostatitis may also increase an individual’s susceptibility to the condition.
Symptoms of Prostatitis
Prostatitis is a urological condition characterized by inflammation of the prostate gland, which can lead to a range of symptoms. The symptoms can vary in severity and type, depending on the specific type of prostatitis and the individual’s health. In this section, we’ll provide a detailed overview of the common symptoms associated with prostatitis:
1. Pelvic Pain and Discomfort:
Pelvic pain is often the most prominent and distressing symptom of prostatitis. It can manifest as a persistent, dull ache or a sharp, stabbing pain in the lower abdomen, groin, lower back, or perineum (the area between the scrotum and the anus).
2. Urinary Symptoms:
Painful or burning sensation during urination. A need to urinate more frequently than usual, including waking up at night to urinate (nocturia). A sudden, strong urge to urinate, sometimes with the feeling that one cannot hold it. A sense of incomplete bladder emptying after urination.
3. Sexual Dysfunction:
Difficulty achieving or maintaining an erection may occur in some cases of prostatitis. Ejaculatory pain is often described as a burning or stinging sensation during or after ejaculation. Decreased sexual desire or interest in sexual activity.
4. Flu-Like Symptoms (Acute Bacterial Prostatitis – ABP):
A high fever, often accompanied by chills and sweating. Generalized muscle pain and weakness. Feeling unusually tired or exhausted.
5. General Symptoms:
- Rectal Pain: Some individuals may experience pain or discomfort when passing stools or during rectal examinations.
- Painful Sitting: Discomfort or pain when sitting for prolonged periods.
- Backache: Lower back pain may accompany pelvic discomfort.
- Abdominal Pain: Some individuals may report pain or discomfort in the lower abdomen.
- Depression and Anxiety: Chronic prostatitis can lead to emotional distress, including symptoms of depression and anxiety.
6. Systemic Symptoms (Severe Cases):
In rare, severe cases of acute bacterial prostatitis, the infection can spread to the bloodstream, leading to a life-threatening condition known as septic shock. Symptoms include rapid breathing, confusion, low blood pressure, and organ failure.
It’s important to note that the specific symptoms and their severity can vary from person to person and depend on the type of prostatitis. For example, acute bacterial prostatitis (ABP) tends to produce more severe symptoms, including fever and chills, while chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) is characterized by persistent pelvic pain and urinary symptoms without the same acute systemic symptoms.
Impact on Male Fertility
Prostatitis, the inflammation of the prostate gland, can have a significant impact on male fertility. While the severity and specific effects can vary depending on the type and duration of prostatitis, as well as individual factors, it’s essential to understand how this condition can affect fertility. In this section, we will explore in detail the impact of prostatitis on male fertility:
1. Disruption of Sperm Production
Prostatitis, particularly chronic forms, can disrupt the normal function of the prostate gland, which plays a crucial role in sperm production and storage. Inflammation or infection of the prostate can lead to impaired sperm production and function.
- Impact: Reduced sperm production can result in a lower sperm count, which is a critical factor in male fertility. Sperm count measures the number of sperm in a semen sample, and a lower count can reduce the chances of successfully fertilizing an egg.
2. Obstructed Ejaculatory Ducts
Inflammation and infection of the prostate can lead to the narrowing or blockage of the ejaculatory ducts. These ducts are responsible for transporting sperm from the testes and seminal vesicles into the urethra during ejaculation.
- Impact: Obstructed ejaculatory ducts can impede the passage of sperm during ejaculation, preventing them from reaching the egg in the female reproductive tract. This obstruction can result in infertility or reduced fertility.
3. Semen Abnormalities
Prostatitis can lead to abnormalities in semen composition, including changes in sperm concentration, motility (ability to swim), and morphology (shape and structure of sperm). These abnormalities can compromise the quality of sperm.
- Impact: Semen abnormalities can significantly impact male fertility. Reduced sperm motility makes it challenging for sperm to reach and penetrate the egg, while abnormalities in sperm morphology can affect their ability to fertilize the egg.
4. Sexual Dysfunction
The pain and discomfort associated with prostatitis can lead to sexual dysfunction, including erectile dysfunction (difficulty achieving or maintaining an erection) and painful ejaculation.
- Impact: Sexual dysfunction can interfere with the ability to engage in sexual intercourse and ejaculate semen containing viable sperm. This can reduce the chances of conception.
5. Psychological Stress
Coping with the physical and emotional toll of prostatitis can lead to stress and anxiety. These psychological factors can further exacerbate sexual dysfunction and impact fertility.
- Impact: Stress and anxiety can have a negative effect on sexual function and overall well-being. They can reduce sexual desire, impair sexual performance, and contribute to fertility-related concerns.
6. Fertility Preservation
For individuals who are concerned about fertility during or after prostatitis treatment, fertility preservation options may be considered. One common approach is sperm banking, which involves storing healthy sperm for future use in assisted reproductive techniques such as in vitro fertilization (IVF).
Management and Treatment
The management and treatment of prostatitis depend on the type and underlying cause of the condition, as well as the severity of symptoms. It’s crucial to consult a healthcare professional for a thorough evaluation and personalized treatment plan. Here, we provide a detailed overview of the management and treatment options for prostatitis:
1. Antibiotics for Bacterial Prostatitis (ABP and CBP)
Bacterial prostatitis, such as acute bacterial prostatitis (ABP) and chronic bacterial prostatitis (CBP), is caused by bacterial infections. Therefore, antibiotics are the primary treatment approach.
- Treatment: A healthcare provider will prescribe antibiotics to target the specific bacteria responsible for the infection. Antibiotics are typically administered for several weeks in the case of CBP. In severe cases of ABP, hospitalization may be required for intravenous antibiotics.
2. Pain Management
Prostatitis can cause significant pain and discomfort, which may require pain management strategies.
- Treatment: Over-the-counter pain relievers like ibuprofen or acetaminophen may be recommended to alleviate mild to moderate pain. For severe pain, prescription pain medications may be prescribed. Heat therapy, such as warm baths or heating pads, can also help relieve pelvic discomfort.
3. Alpha-Blockers
Alpha-blockers are medications that relax the muscles in the prostate bladder and neck, potentially improving urinary symptoms associated with prostatitis.
- Treatment: Alpha-blockers like tamsulosin (Flomax) may be prescribed to reduce urinary symptoms such as hesitancy and incomplete emptying. They can help relieve discomfort during urination.
4. Lifestyle Modifications
Certain lifestyle changes can help manage symptoms and improve overall well-being during prostatitis.
- Treatment: Lifestyle modifications may include:
- Avoiding Trigger Foods: Some individuals find that avoiding spicy foods, caffeine, and alcohol can reduce symptoms.
- Hydration: Maintaining good hydration can help dilute urine and reduce urinary irritation.
- Stress Management: Stress reduction techniques, such as relaxation exercises or counselling, can help manage psychological symptoms.
5. Physical Therapy (CP/CPPS)
Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) may benefit from physical therapy to address muscle tension and dysfunction in the pelvic area.
- Treatment: Pelvic floor physical therapy involves exercises and techniques to relax and strengthen pelvic muscles. A physical therapist with expertise in pelvic floor issues can provide guidance and treatment.
6. Psychological Support
Coping with the physical and emotional impact of prostatitis can lead to stress, anxiety, and depression.
- Treatment: Psychological support, including counselling or support groups, can be valuable in managing stress and emotional well-being during prostatitis. It can also help address any sexual dysfunction-related concerns.
7. Fertility Preservation
If fertility preservation is a concern during or after prostatitis treatment, individuals may consider sperm banking. This process involves storing healthy sperm for future use in assisted reproductive techniques, such as in vitro fertilization (IVF).
Conclusion
The journey through understanding prostatitis and its profound impact on male fertility has taken us into the intricate world of this urological condition. We’ve explored the various types of prostatitis, the factors that contribute to its development, and the myriad of symptoms it can manifest. Moreover, we’ve delved into the intricate ways prostatitis can influence male fertility, from disrupting sperm production and obstructing ejaculatory ducts to causing semen abnormalities and sexual dysfunction.
Our hope is that this comprehensive exploration has not only shed light on the complexities of prostatitis but also empowered you to make informed decisions about your health. Remember, you are not alone on this journey, and there are healthcare professionals ready to assist you in managing and overcoming the challenges of prostatitis, ensuring that your path to fertility remains open and hopeful.
Dr. Sumit Sharma is an experienced urologist, andrologist, and kidney transplant surgeon with over 20 years of clinical experience. He is the founder of the Department of Urology at multiple hospitals in Gurgaon and has established successful kidney transplant programs across the city.



