Imagine your body’s internal filtration system, the kidneys, silently harbouring a genetic time bomb, gradually unleashing its destructive force. This is the eerie reality of Polycystic Kidney Disease (PKD), a hereditary condition that affects countless individuals worldwide. Often described as a “silent killer,” PKD’s symptoms may remain concealed for years, stealthily undermining kidney function until they finally surface. In this blog, we embark on a journey to unravel the mysteries of PKD, exploring its symptoms, uncovering its genetic causes, and shedding light on the various treatment options that offer hope to those living with this enigmatic condition. Join us as we delve into the depths of PKD, a disease that silently reshapes lives.
Understanding of PKD
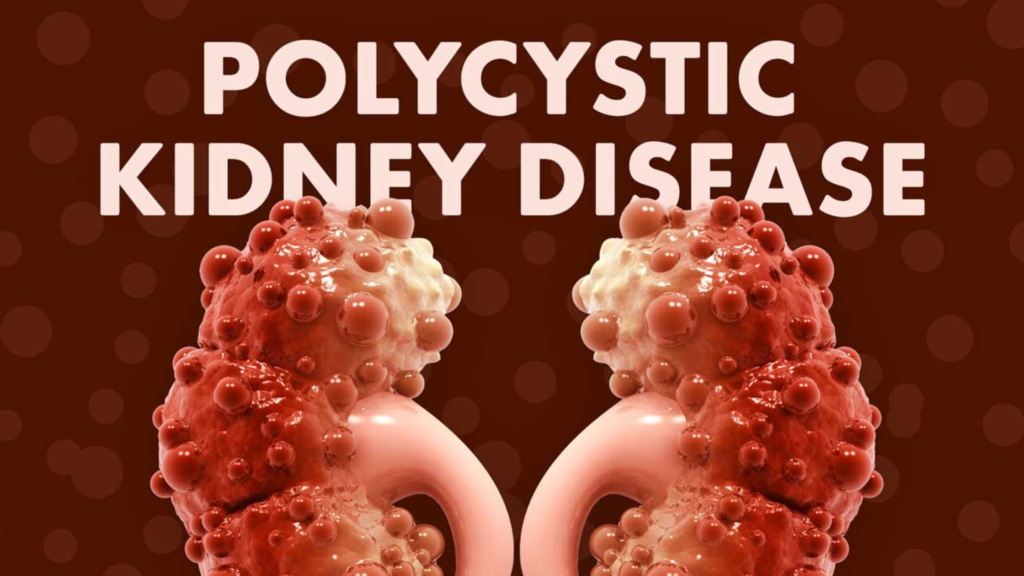
Polycystic Kidney Disease (PKD) is a genetic disorder characterized by the development of fluid-filled sacs or cysts within the kidneys. These cysts gradually replace normal kidney tissue, affecting kidney function and leading to a range of complications. PKD is one of the most common hereditary kidney diseases, and it can be categorized into two main types:
Autosomal Dominant Polycystic Kidney Disease (ADPKD): This is the most prevalent form of PKD, accounting for approximately 90% of cases. ADPKD is inherited in an autosomal dominant manner, which means that an affected individual has a 50% chance of passing the disease to their offspring. Mutations in either the PKD1 or PKD2 genes are responsible for ADPKD. These mutations lead to the formation of cysts in the kidneys, liver, and other organs.
Autosomal Recessive Polycystic Kidney Disease (ARPKD): ARPKD is a rarer form of PKD and is inherited in an autosomal recessive manner. Both parents must carry a copy of the faulty gene for their child to develop the disease. Mutations in the PKHD1 gene primarily cause ARPKD. Unlike ADPKD, which primarily affects adults, ARPKD typically presents in infancy or early childhood and primarily affects the kidneys.
Symptoms of PKD
Abdominal and Lower Back Pain
One of the most common symptoms of PKD is persistent pain in the abdomen and lower back. This pain can vary in intensity from mild discomfort to severe, and it typically results from the expanding cysts. As the cysts grow, they put pressure on the surrounding kidney tissue, which triggers pain. This discomfort can be chronic and is often described as a dull, aching sensation.
Hypertension (High Blood Pressure)
Hypertension, or high blood pressure, is a significant complication of PKD. It affects a substantial number of individuals with the disease. Cysts within the kidneys can lead to the overproduction of hormones that regulate blood pressure, resulting in elevated blood pressure levels. Uncontrolled hypertension can further damage the kidneys and increase the risk of cardiovascular problems, making its early detection and management crucial.
Frequent Urination
PKD can disrupt the normal filtration and concentration processes within the kidneys. As a result, affected individuals may experience an increased need to urinate. This frequent urination can be bothersome and disrupt daily activities, as it often requires frequent trips to the bathroom.
Hematuria (Blood in Urine)
Hematuria, or the presence of blood in the urine, is a concerning symptom of PKD. The cysts within the kidneys can interfere with the filtering process, allowing red blood cells to leak into the urine. This can result in pink, red, or brown urine and is an indicator of kidney damage. Hematuria may be intermittent and can occur alongside other symptoms.
Kidney Stones
PKD increases the risk of developing kidney stones. The presence of cysts can disrupt the normal flow of urine, leading to the accumulation of minerals and substances that can crystallize and form stones. Kidney stones can cause severe pain when they move through the urinary tract, and they may require medical intervention to alleviate symptoms and promote their passage.
Decline in Kidney Function
Over time, as the cysts replace healthy kidney tissue, there is a gradual decline in kidney function. This decline can lead to a range of complications, including kidney failure. As the kidneys lose their ability to effectively filter waste products and regulate fluid and electrolyte balance, individuals may experience symptoms such as fatigue, weakness, oedema (swelling), and imbalances in electrolytes like potassium and sodium.
Diagnosis and Screening
Diagnosing and screening for Polycystic Kidney Disease (PKD) is essential to identify the condition in its early stages and begin appropriate management. Early diagnosis allows for better control of symptoms and complications, helping to preserve kidney function and improve the quality of life for individuals with PKD. Here’s a detailed explanation of the diagnosis and screening processes for PKD
Family History
One of the initial steps in diagnosing PKD is to assess the patient’s family history. Since PKD is a hereditary condition, a family history of the disease is a significant risk factor. If close relatives, such as parents, siblings, or grandparents, have been diagnosed with PKD, this increases the likelihood of an individual being at risk for the disease.
Physical Examination
A physical examination by a healthcare provider may reveal signs of PKD, such as an enlarged or palpable kidney mass, abdominal tenderness, or hypertension. However, PKD is often asymptomatic in its early stages, and physical examination alone may not provide a definitive diagnosis.
Imaging Studies
Imaging studies are a key component of PKD diagnosis. They allow healthcare professionals to visualize the presence of cysts within the kidneys. The most common imaging techniques for PKD diagnosis include:
Ultrasound: Ultrasound is often the initial imaging modality used to screen for PKD. It provides detailed images of the kidneys, showing the presence of cysts and their size.
Computed Tomography (CT) Scan: CT scans offer more detailed and cross-sectional views of the kidneys. They can help confirm the presence of cysts, assess their characteristics, and identify any complications.
Magnetic Resonance Imaging (MRI): MRI can provide detailed images of the kidneys and is particularly useful when radiation exposure needs to be minimised, such as in pregnant individuals.
Genetic Testing
- Genetic testing is the most definitive method for diagnosing PKD and determining the specific genetic mutation responsible for the disease. This testing is particularly valuable when clinical or imaging findings are inconclusive, or to confirm the diagnosis in individuals with a family history of PKD.
- Genetic testing identifies mutations in the PKD1 and PKD2 genes for Autosomal Dominant Polycystic Kidney Disease (ADPKD) and the PKHD1 gene for Autosomal Recessive Polycystic Kidney Disease (ARPKD).
- Genetic testing can be performed through blood or saliva samples, and results help establish a precise diagnosis, enabling genetic counselling for affected individuals and their families.
Blood and Urine Tests
- Blood tests may be ordered to assess kidney function, as PKD can lead to a decline in kidney function over time. Blood tests may measure creatinine levels, glomerular filtration rate (GFR), and other markers of kidney health.
- Urine tests can detect the presence of hematuria (blood in the urine) and proteinuria (elevated levels of protein in the urine), both of which are common in PKD and indicative of kidney damage.
Additional Diagnostic Considerations
- In some cases, additional tests or evaluations may be necessary to assess the extent and impact of PKD, especially if complications are suspected. These can include:
- Evaluation for kidney stones if symptoms suggest their presence.
- Liver imaging, as PKD can lead to the development of liver cysts in some cases.
- Regular monitoring through follow-up imaging studies and blood tests to track the progression of the disease and kidney function.
Early diagnosis and continuous monitoring are crucial in managing PKD effectively. Once diagnosed, individuals can work with healthcare providers to establish a care plan that includes symptom management, blood pressure control, and interventions to prevent complications, ultimately enhancing their quality of life. Dr. Sumit Sharma is the best Urologist in Gurgaon for the treatment of Polycystic Kidney Disease
Treating Polycystic Kidney Disease
Lifestyle Modifications
- Lifestyle modifications can help individuals with PKD manage the disease and maintain their health. Some key lifestyle changes include:
- Blood Pressure Control: Hypertension (high blood pressure) is a common complication of PKD and can accelerate kidney damage. Medications and lifestyle changes, such as reducing salt intake, can help control blood pressure.
- Pain Management: Over-the-counter or prescription pain medications can provide relief from the abdominal and lower back pain often associated with PKD.
- Dietary Adjustments: A diet low in protein and salt may help reduce the strain on the kidneys and lower blood pressure. Avoiding excessive protein can help reduce the accumulation of waste products that the kidneys must filter.
- Hydration: Staying well-hydrated can help prevent the formation of kidney stones, a common complication of PKD.
Medications
- Medications may be prescribed to manage specific symptoms and complications of PKD:
- Pain Relief: Analgesics, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can help alleviate abdominal and lower back pain.
- Blood Pressure Medications: Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) are commonly used to control hypertension in PKD patients. These medications not only lower blood pressure but can also slow the progression of kidney damage.
- Antibiotics: In cases where cysts become infected and lead to kidney infections or abscesses, antibiotics may be necessary to treat the infection and reduce inflammation.
Surgical Interventions
- Surgical procedures may be considered in cases where complications or symptoms are severe:
- Cyst Drainage: In some instances, large or symptomatic cysts may be drained using minimally invasive procedures, such as percutaneous cyst aspiration. This procedure can provide temporary relief from pain and discomfort.
Kidney Transplant
- In advanced stages of PKD, when kidney function deteriorates to the point of kidney failure, kidney transplantation may be necessary. This involves replacing the diseased kidneys with a healthy donor kidney, either from a living or deceased donor. Kidney transplantation can provide individuals with PKD the opportunity for a better quality of life and improved kidney function.
Ongoing Research and Future Treatments
- Research into PKD is ongoing, and there are promising drug therapies in clinical trials that aim to target specific molecular pathways involved in cyst formation. While these treatments are not yet widely available, they offer hope for the future of PKD management. Potential future treatments may focus on slowing or even halting the progression of the disease, addressing the underlying genetic mutations, and minimizing complications.
Conclusion
PKD is a reminder that even within the most complex of genetic puzzles, there’s a path to understanding, managing, and living with the challenges it poses. With early diagnosis, lifestyle adjustments, medications, and surgical interventions, individuals can navigate the PKD journey with resilience and hope.
In the face of PKD’s silent threat, knowledge is our most potent weapon. By raising awareness, seeking support, and staying informed about the latest research, we can empower those affected by PKD and their families. We can also contribute to the ongoing efforts to unlock the secrets of this complex condition and pave the way for a brighter future.
Ultimately, PKD is not just a diagnosis; it’s a journey. A journey filled with courage, resilience, and the unwavering belief that, in the face of life’s challenges, there is always room for hope and healing.
Dr. Sumit Sharma is an experienced urologist, andrologist, and kidney transplant surgeon with over 20 years of clinical experience. He is the founder of the Department of Urology at multiple hospitals in Gurgaon and has established successful kidney transplant programs across the city.
With a commitment to the highest standards, Dr. Sumit Sharma ensures personalized, professional treatment, making your well-being the primary focus. Choose Dr. Sumit Sharma for outstanding Urological care in Gurgaon.
Polycystic Kidney Disease (PKD) – Symptoms, Causes, Treatment
Imagine your body’s internal filtration system, the kidneys, silently harbouring a genetic time bomb, gradually unleashing its destructive force. This is the eerie reality of Polycystic Kidney Disease (PKD), a hereditary condition that affects countless individuals worldwide. Often described as a “silent killer,” PKD’s symptoms may remain concealed for years, stealthily undermining kidney function until they finally surface. In this blog, we embark on a journey to unravel the mysteries of PKD, exploring its symptoms, uncovering its genetic causes, and shedding light on the various treatment options that offer hope to those living with this enigmatic condition. Join us as we delve into the depths of PKD, a disease that silently reshapes lives.
Understanding of PKD
Polycystic Kidney Disease (PKD) is a genetic disorder characterized by the development of fluid-filled sacs or cysts within the kidneys. These cysts gradually replace normal kidney tissue, affecting kidney function and leading to a range of complications. PKD is one of the most common hereditary kidney diseases, and it can be categorized into two main types:
Autosomal Dominant Polycystic Kidney Disease (ADPKD): This is the most prevalent form of PKD, accounting for approximately 90% of cases. ADPKD is inherited in an autosomal dominant manner, which means that an affected individual has a 50% chance of passing the disease to their offspring. Mutations in either the PKD1 or PKD2 genes are responsible for ADPKD. These mutations lead to the formation of cysts in the kidneys, liver, and other organs.
Autosomal Recessive Polycystic Kidney Disease (ARPKD): ARPKD is a rarer form of PKD and is inherited in an autosomal recessive manner. Both parents must carry a copy of the faulty gene for their child to develop the disease. Mutations in the PKHD1 gene primarily cause ARPKD. Unlike ADPKD, which primarily affects adults, ARPKD typically presents in infancy or early childhood and primarily affects the kidneys.
Symptoms of PKD
Abdominal and Lower Back Pain
One of the most common symptoms of PKD is persistent pain in the abdomen and lower back. This pain can vary in intensity from mild discomfort to severe, and it typically results from the expanding cysts. As the cysts grow, they put pressure on the surrounding kidney tissue, which triggers pain. This discomfort can be chronic and is often described as a dull, aching sensation.
Hypertension (High Blood Pressure)
Hypertension, or high blood pressure, is a significant complication of PKD. It affects a substantial number of individuals with the disease. Cysts within the kidneys can lead to the overproduction of hormones that regulate blood pressure, resulting in elevated blood pressure levels. Uncontrolled hypertension can further damage the kidneys and increase the risk of cardiovascular problems, making its early detection and management crucial.
Frequent Urination
PKD can disrupt the normal filtration and concentration processes within the kidneys. As a result, affected individuals may experience an increased need to urinate. This frequent urination can be bothersome and disrupt daily activities, as it often requires frequent trips to the bathroom.
Hematuria (Blood in Urine)
Hematuria, or the presence of blood in the urine, is a concerning symptom of PKD. The cysts within the kidneys can interfere with the filtering process, allowing red blood cells to leak into the urine. This can result in pink, red, or brown urine and is an indicator of kidney damage. Hematuria may be intermittent and can occur alongside other symptoms.
Kidney Stones
PKD increases the risk of developing kidney stones. The presence of cysts can disrupt the normal flow of urine, leading to the accumulation of minerals and substances that can crystallize and form stones. Kidney stones can cause severe pain when they move through the urinary tract, and they may require medical intervention to alleviate symptoms and promote their passage.
Decline in Kidney Function
Over time, as the cysts replace healthy kidney tissue, there is a gradual decline in kidney function. This decline can lead to a range of complications, including kidney failure. As the kidneys lose their ability to effectively filter waste products and regulate fluid and electrolyte balance, individuals may experience symptoms such as fatigue, weakness, oedema (swelling), and imbalances in electrolytes like potassium and sodium.
Diagnosis and Screening
Diagnosing and screening for Polycystic Kidney Disease (PKD) is essential to identify the condition in its early stages and begin appropriate management. Early diagnosis allows for better control of symptoms and complications, helping to preserve kidney function and improve the quality of life for individuals with PKD. Here’s a detailed explanation of the diagnosis and screening processes for PKD
Family History
One of the initial steps in diagnosing PKD is to assess the patient’s family history. Since PKD is a hereditary condition, a family history of the disease is a significant risk factor. If close relatives, such as parents, siblings, or grandparents, have been diagnosed with PKD, this increases the likelihood of an individual being at risk for the disease.
Physical Examination
A physical examination by a healthcare provider may reveal signs of PKD, such as an enlarged or palpable kidney mass, abdominal tenderness, or hypertension. However, PKD is often asymptomatic in its early stages, and physical examination alone may not provide a definitive diagnosis.
Imaging Studies
Imaging studies are a key component of PKD diagnosis. They allow healthcare professionals to visualize the presence of cysts within the kidneys. The most common imaging techniques for PKD diagnosis include:
Ultrasound: Ultrasound is often the initial imaging modality used to screen for PKD. It provides detailed images of the kidneys, showing the presence of cysts and their size.
Computed Tomography (CT) Scan: CT scans offer more detailed and cross-sectional views of the kidneys. They can help confirm the presence of cysts, assess their characteristics, and identify any complications.
Magnetic Resonance Imaging (MRI): MRI can provide detailed images of the kidneys and is particularly useful when radiation exposure needs to be minimised, such as in pregnant individuals.
Genetic Testing
- Genetic testing is the most definitive method for diagnosing PKD and determining the specific genetic mutation responsible for the disease. This testing is particularly valuable when clinical or imaging findings are inconclusive, or to confirm the diagnosis in individuals with a family history of PKD.
- Genetic testing identifies mutations in the PKD1 and PKD2 genes for Autosomal Dominant Polycystic Kidney Disease (ADPKD) and the PKHD1 gene for Autosomal Recessive Polycystic Kidney Disease (ARPKD).
- Genetic testing can be performed through blood or saliva samples, and results help establish a precise diagnosis, enabling genetic counselling for affected individuals and their families.
Blood and Urine Tests
- Blood tests may be ordered to assess kidney function, as PKD can lead to a decline in kidney function over time. Blood tests may measure creatinine levels, glomerular filtration rate (GFR), and other markers of kidney health.
- Urine tests can detect the presence of hematuria (blood in the urine) and proteinuria (elevated levels of protein in the urine), both of which are common in PKD and indicative of kidney damage.
Additional Diagnostic Considerations
- In some cases, additional tests or evaluations may be necessary to assess the extent and impact of PKD, especially if complications are suspected. These can include:
- Evaluation for kidney stones if symptoms suggest their presence.
- Liver imaging, as PKD can lead to the development of liver cysts in some cases.
- Regular monitoring through follow-up imaging studies and blood tests to track the progression of the disease and kidney function.
Early diagnosis and continuous monitoring are crucial in managing PKD effectively. Once diagnosed, individuals can work with healthcare providers to establish a care plan that includes symptom management, blood pressure control, and interventions to prevent complications, ultimately enhancing their quality of life. Dr. Sumit Sharma is the best Urologist in Gurgaon for the treatment of Polycystic Kidney Disease
Treating Polycystic Kidney Disease
Lifestyle Modifications
- Lifestyle modifications can help individuals with PKD manage the disease and maintain their health. Some key lifestyle changes include:
- Blood Pressure Control: Hypertension (high blood pressure) is a common complication of PKD and can accelerate kidney damage. Medications and lifestyle changes, such as reducing salt intake, can help control blood pressure.
- Pain Management: Over-the-counter or prescription pain medications can provide relief from the abdominal and lower back pain often associated with PKD.
- Dietary Adjustments: A diet low in protein and salt may help reduce the strain on the kidneys and lower blood pressure. Avoiding excessive protein can help reduce the accumulation of waste products that the kidneys must filter.
- Hydration: Staying well-hydrated can help prevent the formation of kidney stones, a common complication of PKD.
Medications
- Medications may be prescribed to manage specific symptoms and complications of PKD:
- Pain Relief: Analgesics, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can help alleviate abdominal and lower back pain.
- Blood Pressure Medications: Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) are commonly used to control hypertension in PKD patients. These medications not only lower blood pressure but can also slow the progression of kidney damage.
- Antibiotics: In cases where cysts become infected and lead to kidney infections or abscesses, antibiotics may be necessary to treat the infection and reduce inflammation.
Surgical Interventions
- Surgical procedures may be considered in cases where complications or symptoms are severe:
- Cyst Drainage: In some instances, large or symptomatic cysts may be drained using minimally invasive procedures, such as percutaneous cyst aspiration. This procedure can provide temporary relief from pain and discomfort.
Kidney Transplant
- In advanced stages of PKD, when kidney function deteriorates to the point of kidney failure, kidney transplantation may be necessary. This involves replacing the diseased kidneys with a healthy donor kidney, either from a living or deceased donor. Kidney transplantation can provide individuals with PKD the opportunity for a better quality of life and improved kidney function.
Ongoing Research and Future Treatments
- Research into PKD is ongoing, and there are promising drug therapies in clinical trials that aim to target specific molecular pathways involved in cyst formation. While these treatments are not yet widely available, they offer hope for the future of PKD management. Potential future treatments may focus on slowing or even halting the progression of the disease, addressing the underlying genetic mutations, and minimizing complications.
Conclusion
PKD is a reminder that even within the most complex of genetic puzzles, there’s a path to understanding, managing, and living with the challenges it poses. With early diagnosis, lifestyle adjustments, medications, and surgical interventions, individuals can navigate the PKD journey with resilience and hope.
In the face of PKD’s silent threat, knowledge is our most potent weapon. By raising awareness, seeking support, and staying informed about the latest research, we can empower those affected by PKD and their families. We can also contribute to the ongoing efforts to unlock the secrets of this complex condition and pave the way for a brighter future.
Ultimately, PKD is not just a diagnosis; it’s a journey. A journey filled with courage, resilience, and the unwavering belief that, in the face of life’s challenges, there is always room for hope and healing.
Dr. Sumit Sharma is an experienced urologist, andrologist, and kidney transplant surgeon with over 20 years of clinical experience. He is the founder of the Department of Urology at multiple hospitals in Gurgaon and has established successful kidney transplant programs across the city.
With a commitment to the highest standards, Dr. Sumit Sharma ensures personalized, professional treatment, making your well-being the primary focus. Choose Dr. Sumit Sharma for outstanding Urological care in Gurgaon.