Painful Bladder Syndrome, also known as Interstitial Cystitis (IC), is a chronic condition that causes recurring pain and discomfort in the bladder and pelvic region. It is a complex and poorly understood disorder that primarily affects the bladder but can also impact the surrounding tissues and organs. This blog aims to provide a comprehensive overview of Painful Bladder Syndrome, including its causes, symptoms, and treatment options.
Causes of Painful Bladder Syndrome
The exact cause of Painful Bladder Syndrome is unknown, but several factors have been identified as potential contributors. These include:
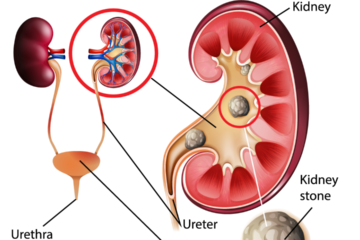
- Bladder lining abnormalities: People with IC may have a defective bladder lining that allows toxic substances in urine to irritate the bladder wall.
- Dysfunction of the pelvic floor muscles: Pelvic floor dysfunction can lead to an abnormal response to bladder filling and contribute to bladder pain and urinary symptoms.
- Autoimmune factors: Some evidence suggests that IC may have an autoimmune component, where the body’s immune system mistakenly attacks the bladder.
- Neurogenic inflammation: Nerves in the bladder may become hypersensitive, leading to chronic pain and increased urgency and frequency of urination.
Symptoms of Painful Bladder Syndrome
The symptoms of Painful Bladder Syndrome can vary from person to person and may range from mild to severe. Common symptoms include:
- Bladder pain: Persistent pain or discomfort in the bladder region, often described as aching, pressure, or burning sensation.
- Increased urinary frequency: A need to urinate more frequently, sometimes as often as every 10-15 minutes.
- Urgency: Strong, sudden urge to urinate that is difficult to delay.
- Painful sexual intercourse: Pain or discomfort during or after sexual activity, known as dyspareunia.
- Pelvic pain: Discomfort or pain in the pelvic region, including the lower abdomen, groin, or perineum.
- Nocturia: Frequent urination at night, disrupting sleep patterns.
Diagnosing Painful Bladder Syndrome
Diagnosing Painful Bladder Syndrome can be challenging as there is no definitive test. A healthcare provider may perform the following to rule out other conditions and arrive at a diagnosis:
- Medical history and symptom assessment: The healthcare provider will inquire about the patient’s symptoms, and medical history, and perform a physical examination.
- Urine tests: A urine sample may be analyzed to check for signs of infection or other abnormalities.
- Cystoscopy: A thin tube with a camera (cystoscope) is inserted into the bladder to visually examine the bladder lining for signs of inflammation or other abnormalities.
- Biopsy: In some cases, a small sample of bladder tissue may be taken for further analysis.
Treatment Options for Painful Bladder Syndrome
While there is no cure for Painful Bladder Syndrome, several treatment options aim to alleviate symptoms and improve the quality of life for affected individuals. These include:
- Lifestyle modifications: Avoiding known triggers such as caffeine, alcohol, spicy foods, and artificial sweeteners can help manage symptoms. Maintaining a healthy diet, managing stress, and practising pelvic floor exercises may also provide relief.
- Medications: Over-the-counter pain relievers, such as non-steroidal anti-inflammatory drugs (NSAIDs), may help alleviate mild pain. For more severe symptoms, prescription medications like antihistamines, tricyclic antidepressants, and bladder instillations (medications directly inserted into the bladder) may be recommended.
- Bladder instillations: Medications, such as dimethyl sulfoxide (DMSO) or a combination of heparin, lidocaine, and sodium bicarbonate, can be instilled into the bladder to reduce inflammation and alleviate symptoms.
- Nerve stimulation: Neuromodulation techniques, such as transcutaneous electrical nerve stimulation (TENS) or sacral nerve stimulation, can help regulate nerve activity and reduce pain.
- Bladder distention: Stretching the bladder by filling it with a liquid can sometimes provide temporary relief from symptoms.
- Physical therapy: Pelvic floor physical therapy, including techniques like biofeedback and pelvic floor muscle relaxation exercises, can help improve muscle coordination and reduce pain.
- Psychological support: Chronic pain conditions like Painful Bladder Syndrome can have a significant impact on mental health. Support from therapists, psychologists, or support groups can help individuals cope with the emotional challenges associated with the condition.
Conclusion
Painful Bladder Syndrome, or Interstitial Cystitis, is a chronic condition that causes recurring pain and discomfort in the bladder and pelvic region. It is important to remember that the experience of Painful Bladder Syndrome can vary from person to person, and treatment plans should be tailored to individual needs. Consulting with a healthcare professional who specializes in urology or pelvic pain can provide guidance, accurate diagnosis, and personalized treatment options to effectively manage the condition.
Living with Painful Bladder Syndrome may present challenges, but with the right support and management strategies, individuals can find ways to alleviate symptoms, improve their quality of life, and regain control over their bladder health. Remember, you are not alone, and there is hope for relief and better days ahead.
Dr. Sumit Sharma is an experienced urologist, andrologist, and kidney transplant surgeon with over 20 years of clinical experience. He is the founder of the Department of Urology at multiple hospitals in Gurgaon and has established successful kidney transplant programs across the city.
Here are some frequently asked questions about Painful Bladder Syndrome:
Q. Is bladder pain curable?
The curability of bladder pain depends on the underlying cause. Bladder pain can be a symptom of various conditions, including urinary tract infections, bladder stones, bladder cancer, and interstitial cystitis (also known as Painful Bladder Syndrome). In some cases, treating the underlying cause can alleviate bladder pain and resolve the issue completely.
For example, if bladder pain is due to a urinary tract infection, appropriate antibiotics can clear the infection and relieve the associated pain. Similarly, if bladder stones are causing pain, removing the stones through procedures like lithotripsy or cystoscopy can provide relief.
However, when it comes to conditions like interstitial cystitis, which is a chronic condition, the pain may not be curable in the traditional sense. Interstitial cystitis is a complex and poorly understood disorder, and there is currently no known cure. The focus of treatment for interstitial cystitis is on managing symptoms and improving the individual’s quality of life.
Various treatment approaches, including lifestyle modifications, medications, bladder instillations, nerve stimulation, physical therapy, and psychological support, can help alleviate bladder pain and manage the symptoms associated with interstitial cystitis. These treatment options aim to provide relief and improve the overall well-being of individuals with the condition, even though a complete cure may not be achievable.
It is essential to consult with a healthcare professional to determine the underlying cause of bladder pain and develop an appropriate treatment plan tailored to individual needs. They can provide a more accurate assessment of the curability and available treatment options based on the specific circumstances.
Q. Who is the best Urologist in Gurgaon?
Dr. Sumit Sharma is an experienced urologist, andrologist, and kidney transplant surgeon with over 20 years of clinical experience. He is the founder of the Department of Urology at multiple hospitals in Gurgaon and has established successful kidney transplant programs across the city.
Q. Does walking help with Bladder pain?
Walking can potentially help alleviate bladder pain for some individuals, but its effectiveness may vary depending on the underlying cause of the pain. Here are a few reasons why walking can be beneficial:
- Increased blood flow: Walking stimulates blood circulation throughout the body, including the pelvic region. Improved blood flow can help reduce inflammation and promote healing in the bladder, potentially relieving pain.
- Stress reduction: Regular exercise, including walking, can help manage stress levels. Stress is known to exacerbate symptoms of bladder pain conditions such as interstitial cystitis. By reducing stress, walking may indirectly alleviate bladder pain and promote overall well-being.
- Pelvic floor muscle engagement: Walking engages the muscles in the pelvic floor, which can help improve muscle tone and coordination. Strong and well-coordinated pelvic floor muscles are essential for bladder control and can contribute to better bladder health and reduced pain.
- Enhanced digestion: Walking aids in maintaining a healthy digestive system. Problems with digestion, such as constipation or bowel irregularities, can impact bladder function and contribute to bladder pain. By promoting regular bowel movements, walking may indirectly improve bladder symptoms.
While walking can have potential benefits for bladder pain, it is important to listen to your body and pay attention to any discomfort during or after exercise. Some individuals with certain conditions, such as interstitial cystitis, may find that high-impact exercises or prolonged walking exacerbate their symptoms. In such cases, it may be helpful to explore other low-impact exercises or work with a healthcare professional or physical therapist to develop an exercise routine tailored to your specific needs.
It’s always advisable to consult with a healthcare professional who can evaluate your individual situation, provide personalized advice, and recommend appropriate exercises or physical activities to manage bladder pain effectively.