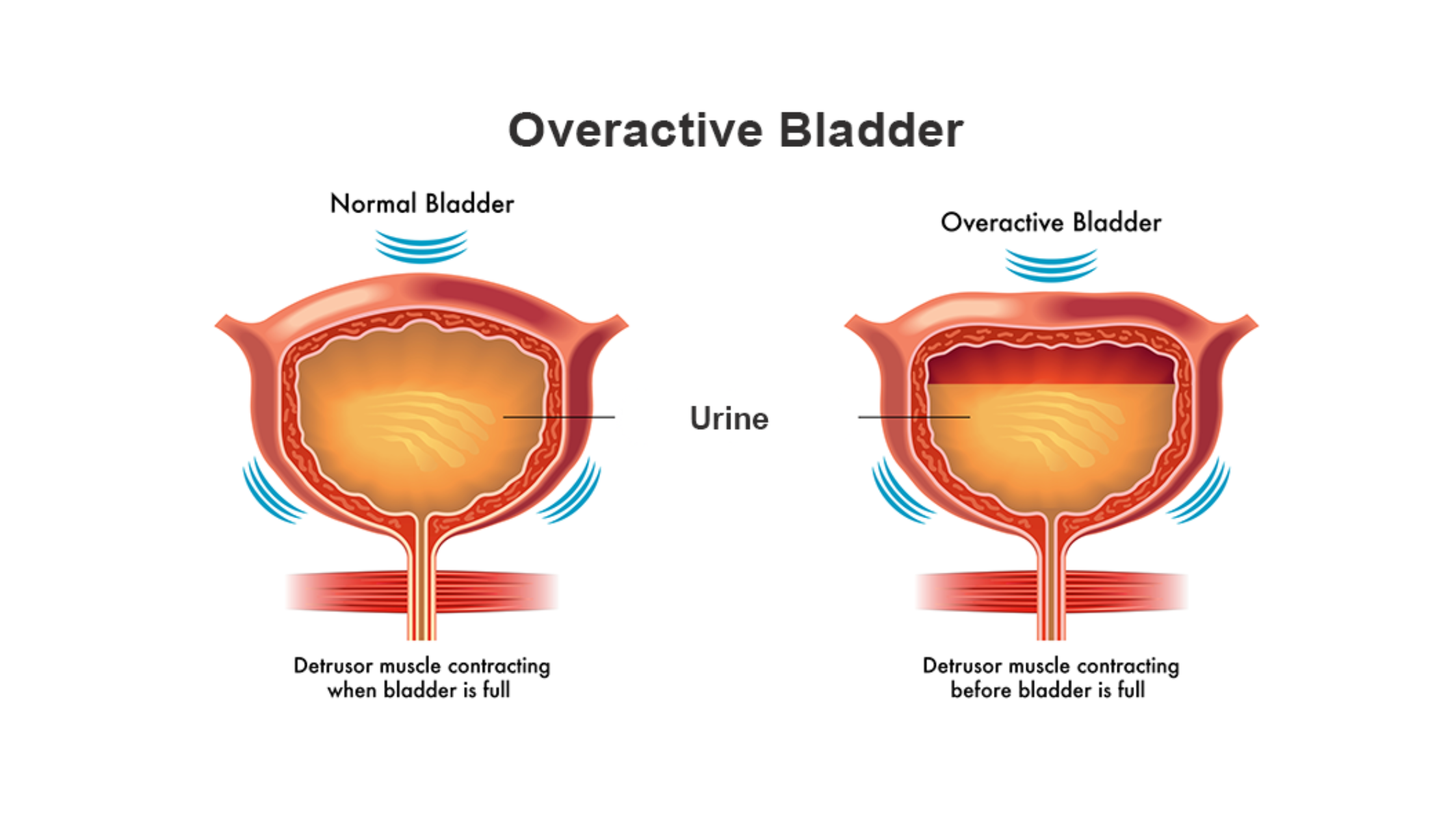
In the complex tapestry of human health, the often unspoken and misunderstood realm of bladder function plays a pivotal role. Overactive Bladder (OAB), a condition affecting millions globally, transcends mere inconvenience to significantly impact the daily lives of those grappling with its symptoms. From the persistent urgency to the challenge of maintaining bladder control, OAB introduces a set of challenges that can, at times, be overwhelming. However, knowledge is a powerful ally, and in this comprehensive blog post, we embark on a journey to unravel the complexities of Overactive Bladder, exploring its causes, understanding its symptoms, and navigating the diverse landscape of treatment options available to reclaim control and enhance the quality of life. Join us as we shed light on this often underestimated aspect of health, empowering individuals with the insights needed to manage and overcome the challenges posed by Overactive Bladder.
Causes of Overactive Bladder (OAB)
Overactive Bladder (OAB) is a complex condition influenced by a variety of factors, both physiological and lifestyle-related. Understanding the underlying causes is crucial for effective management and targeted treatment. Let’s delve into the intricate details of the causes of Overactive Bladder.
- Muscle Weakness or Damage: The bladder relies on a set of muscles to contract and relax properly for effective urination. Weakness or damage to these muscles can disrupt the coordination needed for smooth bladder function.
Contributing Factors: Aging, childbirth, and pelvic surgery can lead to muscle weakening, impacting the bladder’s ability to function optimally.
- Neurological Disorder: The nerves that control bladder function play a vital role in signaling when it’s time to release urine. Neurological disorders can interfere with these signals, causing the bladder to contract involuntarily.
Contributing Factors: Conditions such as multiple sclerosis, Parkinson’s disease, and spinal cord injuries can disrupt nerve communication with the bladder.
- Infections: Infections in the urinary tract can irritate the bladder lining, leading to heightened sensitivity and increased contractions.
Contributing Factors: Untreated or recurrent urinary tract infections (UTIs) can contribute to the development of Overactive Bladder symptoms.
- Bladder Stones: Stones in the bladder can cause irritation and inflammation, triggering Overactive Bladder symptoms.
Contributing Factors: The formation of bladder stones is often linked to mineral imbalances and inadequate fluid intake.
- Medications: Certain medications may have side effects that impact bladder function, leading to symptoms of OAB.
Contributing Factors: Diuretics, sedatives, and medications with anticholinergic effects are known to potentially contribute to OAB symptoms.
- Hormonal Changes: Fluctuations in hormonal levels, particularly in women during menopause, can affect the elasticity of the bladder and its ability to hold urine.
Contributing Factors: Estrogen, a hormone that declines during menopause, plays a role in maintaining the health of the bladder and surrounding tissues.
Symptoms of Overactive Bladder
Overactive Bladder (OAB) manifests through a distinctive set of symptoms, which can significantly impact an individual’s daily life and well-being. Recognizing these symptoms is key to seeking timely medical intervention and formulating an effective management plan. Let’s delve into the detailed explanation of the symptoms associated with Overactive bladder.
Urgency
Urgency is a hallmark symptom of OAB and is characterized by a sudden, compelling need to urinate that may be difficult to control. Individuals with OAB may find themselves rushing to the restroom, often with little warning, and may struggle to delay the urge.
Frequency
Frequent urination is another prevalent symptom, where individuals feel the need to urinate more often than usual, even during times of low fluid intake. Those with OAB may find themselves making multiple trips to the bathroom throughout the day, disrupting normal activities.
Nocturia
Nocturia refers to the need to wake up during the night to urinate, which can disrupt sleep patterns and lead to fatigue. Individuals with OAB may experience multiple episodes of waking up to use the restroom, impacting the overall quality of their sleep.
Incontinence
Incontinence is the involuntary leakage of urine, ranging from mild to severe. OAB can lead to urge incontinence, where the intense urgency to urinate is accompanied by the inability to reach the restroom in time, resulting in leakage.
Hesitancy
Hesitancy is the difficulty in initiating urination, often marked by a delay in the start of the urinary stream. Individuals with OAB may feel a sense of hesitation or difficulty when attempting to urinate, adding to the overall discomfort.
Incomplete Emptying
The sensation of incomplete emptying occurs when individuals feel that their bladder has not fully emptied after urination. Despite urinating, individuals with OAB may still feel a residual fullness in the bladder, leading to a persistent sense of discomfort.
Treatment Options for Overactive Bladder
Managing Overactive Bladder (OAB) involves a multifaceted approach, often tailored to the individual’s specific symptoms and circumstances. Treatment options range from lifestyle modifications and behavioural therapies to medications and, in some cases, surgical interventions. Let’s explore these treatment options in detail:
- Lifestyle Modifications
Fluid Management: Regulating fluid intake, especially reducing caffeine and alcohol consumption, can help alleviate OAB symptoms. Limiting fluids before bedtime may also reduce nocturia.
Bladder Training: Scheduled bathroom breaks and gradually increasing the time between voids can help train the bladder to hold urine for longer periods.
Weight Management: Maintaining a healthy weight can reduce pressure on the bladder and alleviate symptoms.
- Pelvic Floor Exercises
Kegel Exercises: Strengthening the pelvic floor muscles through Kegel exercises can improve bladder control and reduce urgency and leakage.
- Medications
Anticholinergic Medications: Drugs like oxybutynin, tolterodine, and solifenacin work by relaxing bladder muscles, and reducing urgency and frequency.
Beta-3 Agonists: Mirabegron is a medication that relaxes the bladder muscle and increases bladder capacity, offering an alternative to anticholinergic medications.
- Botox Injections
Procedure: Botox can be injected into the bladder muscle, causing temporary paralysis and reducing muscle spasms.
Application: Typically reserved for cases where other treatments have failed, Botox injections provide relief for several months.
- Nerve Stimulation Therapies
Sacral Nerve Stimulation (SNS): This involves the implantation of a device that delivers electrical impulses to the sacral nerves, modulating bladder function.
Percutaneous Tibial Nerve Stimulation (PTNS): A less invasive option involving the stimulation of the tibial nerve through electrodes placed near the ankle.
- Surgical Interventions
Bladder Augmentation: Enlarging the bladder’s capacity by using a portion of the bowel to replace or augment the bladder.
Urinary Diversion: Redirecting urine away from the bladder to reduce symptoms, is often used in severe cases.
- Combination Therapies
Tailored Approaches: Some individuals may benefit from a combination of treatments, such as medications along with behavioural therapies or pelvic floor exercises.
- Biofeedback
Technique: Biofeedback involves using electronic monitoring to help individuals gain awareness and control over pelvic muscles, aiding in symptom management.
- Counselling and Support
Psychological Impact: OAB can have emotional and psychological effects. Counselling and support groups can help individuals cope with the impact of OAB on their daily lives.
Conclusion
Arming ourselves with an understanding of the factors contributing to OAB allows us to navigate its challenges with a sense of purpose and control. Recognising the symptoms, whether it’s the sudden urgency, the persistent frequency, or the emotional toll of incontinence, is the crucial first step toward seeking the support and solutions needed for effective management.
The diverse treatment options available, ranging from lifestyle adjustments and pelvic floor exercises to medications and surgical interventions, underscore the importance of personalized care. What works for one may not be the best fit for another, emphasising the need for a tailored approach guided by healthcare professionals who specialise in urological and pelvic health.
As we wrap up this exploration into Overactive Bladder, we hope that this information serves as a beacon of knowledge and support for those grappling with OAB. Seeking assistance is not a sign of weakness, but rather a testament to resilience and a commitment to regaining a sense of normalcy and control.
Remember, you are not alone on this journey. With the right knowledge, support, and a collaborative approach to healthcare, individuals can reclaim their lives from the clutches of Overactive Bladder. Here’s to a future where the conversation around bladder health is open, the solutions are accessible, and the path to well-being is paved with understanding and support.
Dr. Sumit Sharma is an experienced urologist, andrologist, and kidney transplant surgeon with over 20 years of clinical experience. He is the founder of the Department of Urology at multiple hospitals in Gurgaon and has established successful kidney transplant programs across the city.
With a commitment to the highest standards, Dr. Sumit Sharma ensures personalised, professional treatment, making your well-being the primary focus. Choose Dr. Sumit Sharma for outstanding Urological care in Gurgaon.