When it comes to family planning, many couples and individuals choose vasectomy as a reliable method of contraception. Vasectomy, a surgical procedure that blocks or severs the vas deferens, offers a permanent solution for those looking to prevent future pregnancies. However, life is known for its twists and turns, and what might have been a firm decision at one point can evolve over time. This leads to a common question: Are vasectomies reversible? In this blog post, we’ll delve into this intriguing topic, discussing the potential for reversing vasectomies, the procedures involved, success rates, and important considerations for those who find themselves contemplating this possibility.
Understanding Vasectomy
Before delving into the reversibility of vasectomies, let’s take a quick look at what a vasectomy entails. A vasectomy is a simple surgical procedure performed under local anaesthesia, typically as an outpatient procedure. During a vasectomy, the surgeon cuts, seals, or blocks the vas deferens to prevent sperm from mixing with semen, effectively preventing pregnancy. It’s essential to note that a vasectomy should be considered a permanent form of contraception, as it is intended to be irreversible. However, advancements in medical technology have made it possible to attempt to reverse the procedure in some cases.
The Vasectomy Reversal Procedure
Vasectomy reversal, medically referred to as vasovasostomy, is a surgical procedure designed to restore fertility in men who have previously undergone a vasectomy. While a vasectomy is considered a permanent form of contraception, advances in medical techniques have made it possible to attempt to reverse the procedure for those who have had a change of heart or circumstances. In this section, we will provide a detailed explanation of the vasectomy reversal procedure, including its techniques, steps, and considerations.
1. Preoperative Evaluation
Before undergoing a vasectomy reversal, a comprehensive evaluation is essential. This includes a thorough medical history review, physical examination, and potentially fertility testing for both partners. The surgeon will assess factors such as the length of time since the vasectomy, the method used for the vasectomy, the presence of scar tissue, and the overall health of the patient.
2. Anesthesia
Vasectomy reversal is typically performed under general anaesthesia. This ensures that the patient is comfortable and pain-free throughout the procedure. The use of anaesthesia also allows the surgeon to perform delicate and precise manoeuvres without causing discomfort to the patient.
3. Incision
The surgeon makes a small incision in the scrotum to access the vas deferens. The location of the incision may vary based on the surgeon’s preference and the patient’s anatomy.
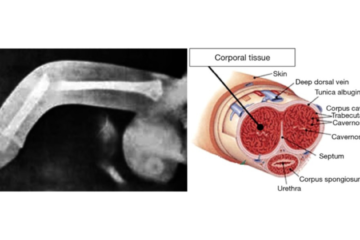
4. Identification and Isolation of Vas Deferens
Once the incision is made, the surgeon carefully identifies and isolates the vas deferens. This is the same tube that was severed or blocked during the initial vasectomy.
5. Vasovasostomy Technique
The vasovasostomy technique involves reconnecting the two cut ends of the vas deferens. The surgeon uses microsurgical techniques to meticulously align the ends of the vas deferens and sutures them together using very fine stitches. The goal is to establish a clear pathway for sperm to travel from the testicles to the ejaculatory ducts once again.
6. Vasoepididymostomy Technique
In cases where there is a blockage closer to the testicles or the vas deferens is damaged, the surgeon may opt for a more complex technique known as vasoepididymostomy. This involves creating a connection between the vas deferens and the epididymis, a small coiled tube located on the back of the testicle. This technique allows sperm to bypass the blockage and flow directly into the reproductive tract.
7. Microsurgical Precision
Microsurgical instruments and techniques are crucial during vasectomy reversal. The surgeon uses a high-powered microscope to magnify the surgical area, enabling precise suturing and minimizing the risk of tissue damage. The delicate nature of the procedure requires steady hands and exceptional surgical skills.
8. Closure
After the reconnection is successfully established, the surgeon closes the incision using sutures that dissolve over time. The scrotal area is dressed, and the patient is monitored in the recovery room before being allowed to return home.
Recovery and Follow-Up
The recovery period following a vasectomy reversal varies, but most patients can expect some discomfort, swelling, and bruising in the scrotal area. Pain medication and proper rest are typically recommended. Patients are advised to avoid strenuous activities and sexual intercourse for several weeks to allow for proper healing.
Success Rates and Factors Influencing Reversal
The success of a vasectomy reversal is influenced by a variety of factors, including the time since the original vasectomy, the specific surgical technique used, the surgeon’s skill, and the overall health of the patient. Understanding these factors can provide valuable insights into the potential outcomes of a vasectomy reversal procedure. In this section, we will explore in detail the factors that can impact the success rates of vasectomy reversal.
1. Time Since Vasectomy
One of the most critical factors affecting the success of a vasectomy reversal is the time that has elapsed since the original vasectomy. Generally, the success rates of reversal tend to be higher when the procedure is performed sooner after the vasectomy. Success rates are notably higher within the first three to five years after the vasectomy. As time progresses, the chances of successful sperm return decrease, partly due to the development of scar tissue or anti-sperm antibodies.
2. Type of Vasectomy
The type of vasectomy originally performed can also influence the success of the reversal. Vasectomies that involve simple techniques like using clips or rings to block the vas deferens are generally more likely to be reversible. In these cases, the surgeon may be able to easily reconnect the vas deferens. However, if a more complex technique was used, such as the removal of a portion of the vas deferens, the chances of successful reversal may be lower due to limited remaining vas deferens.
3. Surgical Skill and Technique
The expertise of the surgeon performing the vasectomy reversal is a crucial factor in determining the success of the procedure. Microsurgical skills are essential for delicate and precise suturing, especially when dealing with structures as small as the vas deferens. Surgeons experienced in microsurgery techniques are better equipped to handle the intricacies of the procedure and optimize the chances of success.
4. Presence of Scar Tissue
Scar tissue formation, known as fibrosis, can occur as a result of the original vasectomy or subsequent infections. This scar tissue can complicate the reconnection process during a reversal. The extent of scar tissue and its location within the vas deferens can impact the difficulty of the procedure and potentially lower the success rates.
5. Anti-Sperm Antibodies
Following a vasectomy, some men may develop antibodies against their own sperm, making them less effective in fertilizing an egg. These anti-sperm antibodies can interfere with the success of a vasectomy reversal by reducing the functionality of the reconnected vas deferens.
6. Age and Partner’s Fertility
The age of the patient and the fertility of the partner also play a role in the success of vasectomy reversal. If the female partner has age-related fertility issues or other reproductive health concerns, even a successful reversal might not lead to a pregnancy. Additionally, advancing age in men can lead to a natural decline in sperm quality and quantity, potentially affecting the chances of successful fertilization.
7. Overall Health and Lifestyle
The general health and lifestyle choices of the patient can indirectly impact the success of a vasectomy reversal. A healthy lifestyle, including proper nutrition, exercise, and avoiding smoking or excessive alcohol consumption, can contribute to better reproductive health and potentially improve the outcomes of the procedure.
Considerations and Alternatives
While vasectomy reversal can be a promising option for individuals and couples who wish to regain their fertility after a vasectomy, it’s important to carefully consider various factors before making a decision. Additionally, there are alternative approaches to achieving pregnancy that should be explored. In this section, we will delve into the key considerations and alternatives that individuals and couples should take into account when contemplating a vasectomy reversal.
Considerations:
Motivation and Emotional Readiness: Before undergoing a vasectomy reversal, individuals and couples should assess their motivations and emotional readiness for expanding their family. A candid discussion about expectations, desires, and potential challenges is crucial to ensure that both partners are on the same page.
Success Rates and Realistic Expectations: Understanding the success rates of vasectomy reversal is vital. While advancements have improved the odds, there is no guarantee of success. Having realistic expectations and being prepared for the possibility of needing additional fertility interventions is important.
Financial Considerations: Vasectomy reversal can be a costly procedure, and it’s essential to consider the financial implications. Factors such as surgical fees, anaesthesia, facility costs, and potential follow-up procedures should all be taken into account.
Health and Age: The overall health and age of both partners can influence the success of a vasectomy reversal and subsequent pregnancy. Advanced age can impact fertility, and underlying health conditions might affect surgical outcomes.
Partner’s Fertility and Reproductive Health: The fertility and reproductive health of the female partner are significant considerations. If the female partner has fertility issues or reproductive health concerns, a vasectomy reversal might not lead to a successful pregnancy.
Alternatives:
In Vitro Fertilization (IVF): IVF is an alternative method to achieve pregnancy when vasectomy reversal is not feasible or successful. In IVF, eggs are retrieved from the female partner and fertilized with sperm in a laboratory setting. The resulting embryos are then transferred to the uterus. IVF offers a higher level of control over conception and can be particularly helpful for couples facing female infertility factors.
Sperm Retrieval Techniques: In cases where vasectomy reversal is not possible or successful, sperm can be directly retrieved from the testicles using techniques such as microsurgical sperm aspiration (MESA) or percutaneous epididymal sperm aspiration (PESA). These retrieved sperm can then be used in conjunction with IVF.
Donor Sperm: Donor sperm can be considered if other options are not viable. Using donor sperm can allow couples to achieve pregnancy even when the male partner’s sperm is unavailable or of poor quality.
Adoption and Surrogacy: For couples who are unable to conceive using their own gametes, adoption or surrogacy can be emotionally rewarding alternatives to biological parenthood.
Conclusion
In the journey of family planning, the question of whether vasectomies are reversible opens up a world of possibilities. Vasectomy reversal, though a complex and delicate procedure, has emerged as a beacon of hope for individuals and couples who find themselves desiring to regain their fertility. As we’ve explored the intricacies of the procedure, factors influencing success, and important considerations, it becomes clear that the decision to pursue a vasectomy reversal is a deeply personal one, requiring careful thought, emotional readiness, and expert guidance.
As you stand at this crossroads, remember that you’re not alone. Seeking counsel from medical professionals who specialize in reproductive health can provide invaluable insights, guiding you toward the choice that aligns best with your aspirations, circumstances, and dreams. Whatever path you embark upon, it’s a journey filled with courage, determination, and the unwavering pursuit of life’s most profound and beautiful experiences – creating and nurturing a family that reflects your unique love and story.
Whether you choose vasectomy reversal or explore alternative avenues, may your journey be marked by resilience, support, and the joy that comes from making decisions that resonate deeply with your heart.
Dr. Sumit Sharma is an experienced and best urologist, andrologist, and kidney transplant surgeon with over 20 years of clinical experience. He is the founder of the Department of Urology at multiple hospitals in Gurgaon and has established successful kidney transplant programs across the city.